Milica Radisic, Ph.D.
AIMBE College of Fellows Class of 2015 In recognition of her innovative research on the design and laboratory development of heart tissue
Skin-care product based on U of T Engineering research donated to health-care workers fighting COVID-19
Via University of Toronto | October 13, 2020 A U of T Engineering spinoff company has donated its entire stock of skin-care product to health-care workers fighting the global pandemic.
A U of T Engineering spinoff company has donated its entire stock of skin-care product to health-care workers fighting the global pandemic.
Several years ago, Professor Milica Radisic (BME, ChemE) and her team developed a peptide-hydrogel biomaterial that prompts skin cells to “crawl” toward one another. The material was initially designed to help close the chronic, non-healing wounds often associated with diabetes, such as bed sores and foot ulcers.
Shortly thereafter, the technology was spun out into Quthero, Inc. a company with offices in Toronto and Pinecrest, Fla. Their first product, Kerra, incorporates the peptides designed by Radisic and her team, and is bioengineered to protect skin from everyday environmental stresses… Continue reading.
Professor Milica Radisic named a YWCA Toronto Woman of Distinction
Via University of Toronto | March 8, 2018Professor Milica Radisic (IBBME, ChemE) has been named a YWCA Toronto Woman of Distinction for 2018. This prestigious recognition honours the outstanding achievements of those who work to improve the lives of women and girls in their community.
Professor Radisic is the Canada Research Chair in Functional Cardiovascular Tissue Engineering and Associate Chair, Research for the Department of Chemical Engineering & Applied Chemistry. She has made transformational advances in tissue engineering which have resulted in new methods for growing human tissue in the lab. Radisic was the first in the world to use electrical impulses and specially designed bioreactors to guide isolated heart cells to assemble into a beating structure. She has also created an injectable tissue patch that could help repair hearts, livers or other organs damaged by disease or injury, as well as the AngioChip, an artificial 3D beating heart tissue. Radisic’s technologies are the basis for two startup companies, both led by women CEOs… Continue reading.
Professor Milica Radisic receives the Steacie Prize
Via University of Toronto | December 18, 2017Professor Milica Radisic (IBBME, ChemE) has been named the 2017 recipient of the Steacie Prize, awarded each year to one engineer or scientist 40 years of age or younger who has made notable contributions to research in Canada. The prize is administered by the E.W.R. Steacie Memorial Fund, a private foundation dedicated to the advancement of Canadian science and engineering.
As the Canada Research Chair in Functional Cardiovascular Tissue Engineering, Professor Radisic has made transformational advances in tissue engineering resulting in new methods for growing human tissue in the lab. Radisic was the first in the world to use electrical impulses and specially designed bioreactors to guide isolated heart cells to assemble into a beating structure. These beating heart tissues are already being used to test potential drugs for side effects… Continue reading.
Milica Radisic Named Fellows of the Royal Society of Canada
Via University of Toronto | September 7, 2017Professors Reza Iravani (ECE) and Milica Radisic (IBBME/ChemE) have been elected fellows of the Royal Society of Canada (RSC) on the basis of their exceptional contributions to scholarship in their fields.
The RSC’s mission is to recognize scholarly, research and artistic excellence, to advise governments and organizations, and to promote a culture of knowledge and innovation in Canada. Fellowship in the RSC is one of the highest honours a Canadian researcher can achieve. New fellows will be inducted at the Society’s Celebration of Excellence in Winnipeg, Manitoba on November 24, 2017.
“Professors Iravani and Radisic’s pioneering research contributions have established them as leaders in their fields, both in Canada and globally,” said Dean Cristina Amon. “They exemplify the very best of engineering innovation and the tremendous calibre of research conducted at U of T Engineering. On behalf of the Faculty, I congratulate them on this richly deserved honour… Continue reading.
Injectable Tissue Patch Could Help Repair Damaged Organs
Via University of Toronto | August 14, 2017A team of U of T Engineering researchers is mending broken hearts with an expanding tissue bandage a little smaller than a postage stamp.
Repairing heart tissue destroyed by a heart attack or medical condition with regenerative cells or tissues usually requires invasive open-heart surgery. But now biomedical engineering Professor Milica Radisic (IBBME, ChemE, Toronto General Hospital Research Institute) and her colleagues have developed a technique that lets them use a small needle to inject a repair patch, without the need to open up the chest cavity.
Radisic’s team are experts in using polymer scaffolds to grow realistic 3D slices of human tissue in the lab. One of their creations, AngioChip, is a tiny patch of heart tissue with its own blood vessels — the heart cells even beat with a regular rhythm. Another one of their innovations snaps together like sheets of Velcro™.
Such lab-grown tissues are already being used to test potential drug candidates for side effects, but the long-term goal is to implant them back into the body to repair damage.
“If an implant requires open-heart surgery, it’s not going to be widely available to patients,” says Radisic. She says that after a myocardial infarction — a heart attack — the heart’s function is reduced so much that invasive procedures like open-heart surgery usually pose more risks than potential benefits. “It’s just too dangerous,” she says… Continue reading.
Skin Cells ‘crawl’ Together To Heal Wounds Treated With Unique Hydrogel Layer
Via U. Toronto | December 14, 2016Time may not heal all wounds, but a proprietary mix of peptides and gel developed by U of T Engineering researchers heals most.
A team led by Professor Milica Radisic (IBBME, ChemE) has demonstrated for the first time that their peptide-hydrogel biomaterial prompts skin cells to “crawl” toward one another, closing chronic, non-healing wounds often associated with diabetes, such as bed sores and foot ulcers.
The team tested their biomaterial on healthy cells from the surface of human skin, called keratinocytes, as well as on keratinocytes derived from elderly diabetic patients. They saw non-healing wounds close 200 per cent faster than with no treatment, and 60 per cent faster than treatment with a leading commercially used collagen-based product.
“We were happy when we saw the cells crawl together much faster with our biomaterial, but if it didn’t work with diabetic cells, that would have been the end of the story,” says Radisic. “But even the diabetic cells travelled much faster — that’s huge.”
Until now, most treatments for chronic wounds involved applying topical ointments that promote the growth of blood vessels to the area. But in diabetic patients, blood vessel growth is inhibited, making those treatments ineffective. Radisic and her team have been working with their special peptide — called QHREDGS, or Q-peptide for short — for almost 10 years. They knew it promoted survival of many different cell types, including stem cells, heart cells and fibroblasts (the cells that make connective tissues), but had never applied it to wound healing.
“We thought that if we were able to use our peptide to both promote survival and give these skin cells a substrate so they could crawl together, they would be able to close the wound more quickly,” says Radisic. “That was the underlying hypothesis.”
U of T Engineering Professor Inducted into Canadian Academy of Engineering
Via U. Toronto | June 27, 2016Milica Radisic is an international leader in the field of cardiovascular tissue engineering. She has pioneered the technique of electrical field stimulation for cultivation of functional heart tissue in the laboratory, leading to innovative new approaches to testing drugs in vitro on arrays of human tissues. Radisic’s groundbreaking research on the design and development of bioreactors for cardiac tissue engineering based on stem cell derived cardiomyocytes and biomaterials has led to accolades such as the NSERC E.W.R. Steacie Fellowship, the Engineers Canada Young Engineer Award, induction into the Royal Society of Canada’s College of New Scholars, Artists and Scientists, and inclusion as one of MIT Technology Review’s Top 35 Innovators under 35.
CREATE Grants Boosts U of T Engineering Research
Via U. Toronto | April 14, 2016Two collaborative research programs led by U of T Engineering professors have received major grants from the Natural Sciences and Engineering Research Council. The funding will help train a new generation of experts in leading edge technologies, from more efficient data transfers for cloud computing to new treatments for disease based on lab-grown human tissues.
Radisic and her team focus on growing human tissues outside the body. They recently unveiled the AngioChip, a system for growing realistic vascularized heart and liver tissues in the lab. These engineered tissues offer an effective way to test potential drug molecules and determine their effect on these organs, an application that is already being commercialized through the spin-off company TARA Biosystems. Eventually, they could be implanted into the body to repair or replace damaged organs.
The new funding will leverage the success of AngioChip’s commercialization. “In contrast to other CREATE programs that provide training through industrial internships, our training here will focus on developing a company,” said Radisic. “Our students will learn how to apply for patents, develop a business plan, make an effective fundraising pitch and more.”
Human-Powered Vehicles and Tissue Engineering
Via U. Toronto | April 1, 2016Professor Milica Radisic (IBBME, ChemE) shared several discoveries from her lab, including a new scaffold that supports the growth of realistic heart and liver tissues outside the body. Such tissues provide an ideal platform for testing new drugs for side effects, but the hope is that one day they will allow for the replacement of damaged human organs. “Organ regeneration is certainly something we will achieve in the future,” said Radisic.
‘Person-on-a-chip’ — U of T engineers Create Lab-Grown Heart and Liver Tissue for Drug Testing and More
Via U. Toronto | March 7, 2016Researchers at U of T Engineering have developed a new way of growing realistic human tissues outside the body. Their “person-on-a-chip” technology, called AngioChip, is a powerful platform for discovering and testing new drugs, and could eventually be used to repair or replace damaged organs.
Professor Milica Radisic (IBBME, ChemE), graduate student Boyang Zhang and their collaborators are among those research groups around the world racing to find ways to grow human tissues in the lab, under conditions that mimic a real person’s body. They have developed unique methods for manufacturing small, intricate scaffolds for individual cells to grow on. These artificial environments produce cells and tissues that resemble the real thing more closely than those grown lying flat in a petri dish.
Lab-Grown Heart Cells To Improve Drug Safety
Via U. Toronto | February 22, 2016Under a microscope at U of T Engineering, heart cells are pulsing together in a petri dish. For Professor Milica Radisic (IBBME, ChemE) and her team, it’s just another day in the lab.
Although they are grown outside the body, the human tissues engineered in Radisic’s lab look and behave just like the real thing. Now, thanks to a new startup company co-founded by Radisic, they are helping drug companies test their products for dangerous side effects.
Testing on lab-grown tissues is one way for pharmaceutical companies to get detailed information on how a drug will perform in the body before proceeding to clinical trials. It avoids many of the ethical issues associated with animal testing and is also much less costly. The hope is that by flagging negative side effects early in the testing process, the new method will help companies avoid the prospect of a drug withdrawals.
One well-known example is the case of Vioxx (also known as rofecoxib), a drug widely used to treat chronic pain. In 2004, Vioxx was withdrawn from the market over concerns about its connection to increased risk of heart attack and stroke. “The company set up a $5-billion fund to compensate people, but there were about 27,000 deaths,” says Radisic. “You can’t measure that with money.”
New “Tissue Velcro” Could Help Repair Damaged Hearts
Via U. Toronto | August 28, 2015Engineers at the University of Toronto just made assembling functional heart tissue as easy as fastening your shoes. The team has created a biocompatible scaffold that allows sheets of beating heart cells to snap together just like Velcro™.
“One of the main advantages is the ease of use,” says Professor Milica Radisic (ChemE, IBBME), who led the project. “We can build larger tissue structures immediately before they are needed, and disassemble them just as easily. I don’t know of any other technique that gives this ability.”
Growing heart muscle cells in the lab is nothing new. The problem is that too often, these cells don’t resemble those found in the body. Real heart cells grow in an environment replete with protein scaffolds and support cells that help shape them into long, lean beating machines. In contrast, lab-grown cells often lack these supports, and tend to be amorphous and weak. Radisic and her team focus on engineering artificial environments that more closely imitate what cells see in the body, resulting in tougher, more robust cells.
Milica Radisic, Ph.D. To be Inducted into Medical and Biological Engineering Elite
Via AIMBE | March 5, 2015WASHINGTON, D.C.— The American Institute for Medical and Biological Engineering (AIMBE) has announced the pending induction of Milica Radisic, Ph.D., Professor, Institute of Biomaterials and Biomedical Engineering, University of Toronto, to its College of Fellows. Dr. Radisic was nominated, reviewed, and elected by peers and members of the College of Fellows In recognition of her innovative research on the design and laboratory development of heart tissue.
With Wires and Electrodes, Tara Bio Builds a Heart on a Chip
Via Xconomy | November 12, 2014It’s been pretty clear for some time that there’s a big need to improve the efficiency of drug R&D. By industry’s count, drugs cost over $1 billion to develop, and most of them fail. A big reason why is the preclinical studies in petri dishes and animals don’t accurately predict how a drug will behave in humans.
That problem has prompted a slew of companies to innovate new ways to test drugs in a more human-representative fashion, and perhaps even change how preclinical testing is done. The latest to come along is Tara Biosystems, a New York-based Columbia University spinout whose founders say they’ve found a novel, stem-cell based approach that can simulate how a human heart would react to a drug.
Tara recently started up with the help of seed funding from New York-based Harris & Harris Group (NASDAQ: TINY), a publicly-traded venture firm that invests in early-stage companies. Misti Ushio, a managing director and executive VP of Harris & Harris, is leading the company, which is being incubated within the firm.
Regulatory filings show that Harris & Harris has invested around $300,000 in Tara. Ushio says the seed funding gives the company about a year’s worth of runway to prove itself—to validate its technology, convince pharmaceutical companies of its worth, and essentially earn an additional investment, like a full-fledged Series A round.
Tara is based on the work of two researchers: Columbia professor Gordana Vunjak-Novakovic and University of Toronto professor Milica Radisic. They met several years ago at Bob Langer’s lab at MIT and have since worked together to turn stem cells into mature heart tissue that can be tested as if it were an adult heart.
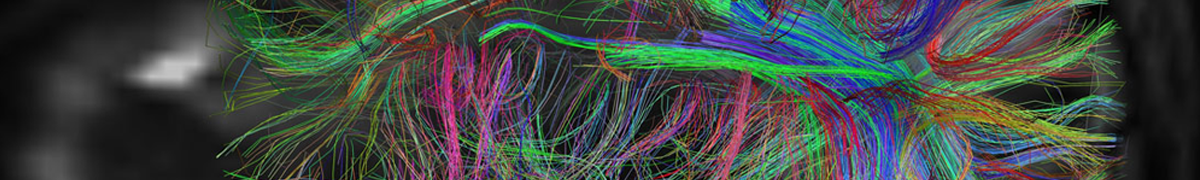
At the core of Tara’s technology are what the founders call “biowire.” Two parallel polymer wires are attached to the wells of a 96-well microplate (pictured above), a common piece of research equipment; the wells function as small test tubes.
The idea is that a researcher would put stem cells into the wells, and then mature them with the help of electrical stimulation. The stem cells grab on to the polymer wires and grow across them as they mature, eventually forming what amounts to tiny micro-hearts, with all of the different cell types that constitute adult heart tissue. Those tiny hearts beat, and pull on the wires when they do. The wires allow for tension, which is important, because by measuring how those wires move, a researcher could determine how the heart contracts, and what, specifically, is causing it to contract in the way it does.
Six Ways U Of T Researchers Are Engineering Your Health
Via U. of Toronto | October 30, 2014Like a scene lifted from Frankenstein, Professor Milica Radisic’s (IBBME, ChemE) “biowire” platform treats immature human cardiac cells, derived from stem cells, to cycles of electric pulses—a process that encourages growth at the same rate as a developing fetus. The result: mature heart tissue that meets a major need in the pharma industry, which, until now, has been unable to test medications on live human heart tissue. Grown along sutures, the heart tissue may also eventually be developed as cardiac patches that, derived from a patient’s own cells, won’t cause rejection issues. Radisic is currently developing the commercial possibilities of this remarkable technology.
 AIMBE
AIMBE
