Xavier Intes, Ph.D.
AIMBE College of Fellows Class of 2016 For outstanding contributions to Biophotonics through the development of innovative functional and molecular optical imaging techniques in industry and academia
Brain-NET predicts surgeons’ capabilities based on neuroimaging data
Via Health Imaging | August 14, 2020A new deep learning approach can pull brain optical imaging data to accurately predict how proficient a physician’s surgical motor skills are, Rensselaer Polytechnic Institute researchers recently reported.
Brain-NET, as it’s known, is the work of engineers at the Troy, New York, institution, and surgery experts from the University at Buffalo Jacobs School of Medicine & Biomedical Sciences.
According to a new study published in IEEE Transactions on Biomedical Engineering, the artificial intelligence was quicker and more accurate than traditional prediction models, most notably when tested using larger datasets… Continue reading.
New Imaging Technique Enables the Study of 3D Printed Brain Tumors
Via Rensselaer Polytechnic Institute | March 31, 2020Glioblastomas are complex, fast-growing malignant brain tumors that are made up of various types of cells. Even with aggressive treatment — which often includes surgery, radiation, and chemotherapy — glioblastomas are difficult to treat, leading to an average survival of 11-15 months.
In research published today in Science Advances, Xavier Intes, a professor of biomedical engineering at Rensselaer, joined a multidisciplinary team from Northeastern University and the Icahn School of Medicine at Mount Sinai to demonstrate a methodology that combines the bioprinting and imaging of glioblastoma cells in a cost-effective way that more closely models what happens inside the human body… Continue reading.
Neural network improves imaging technique for an advanced look at cancer cells
Via Health Imaging | November 13, 2019A new imaging technique developed by researchers from Rensselaer Polytechnic Institute offers a unique look at cells and tissue.
The novel method uses a deep neural network to improve fluorescence lifetime imaging, which allowed scientists at the Troy, New York-based institution to view molecular-level interactions within cells, and may improve doctors’ ability to identify cancer and other diseases.
“This is an enabling technology for many clinical applications,” Xavier Intes, PhD, lead researcher and a professor of biomedical engineering at Rensselaer, said in a statement. “For instance, it may be used for in vivo real-time imaging of a tumor, which may help surgeons see the lesion during their procedures, enabling them to completely remove cancer tissue with minimal damage to healthy tissue… Continue reading.
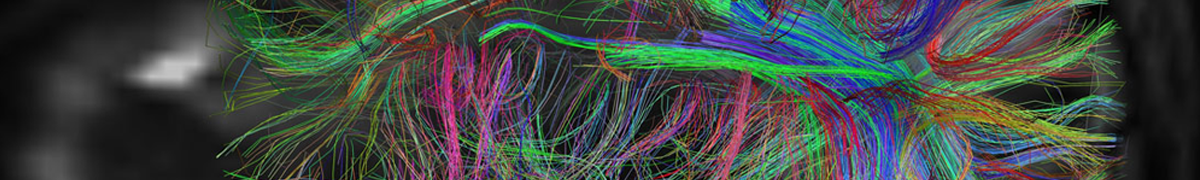
Noninvasive brain imaging shows readiness of trainees to perform operations
Via Eurek Alert | October 24, 2017While simulation platforms have been used to train surgeons before they enter an actual operating room (OR), few studies have evaluated how well trainees transfer those skills from the simulator to the OR. Now, a study that used noninvasive brain imaging to evaluate brain activity has found that simulator-trained medical students successfully transferred those skills to operating on cadavers and were faster than peers who had no simulator training.
The study, led by Arun Nemani, MS, a PhD candidate at Rensselaer Polytechnic Institute in Troy, N.Y., evaluated the surgical proficiency of 19 medical students, six of whom practiced cutting tasks on a physical simulator, eight of whom practiced on a virtual simulator, and five of whom had no practice. Study results were presented at American College of Surgeons Clinical Congress 2017.
…
Study coauthors are Clairice Cooper, MD, and Steven D. Schwaitzberg, MD, FACS, of the University at Buffalo School of Medicine and Biomedical Sciences; and Xavier Intes, PhD, and Suvranu De, PhD, of Rensselaer Polytechnic Institute, Troy… Continue reading.
Xavier Intes, Ph.D. To be Inducted into Medical and Biological Engineering Elite
Via AIMBE | January 20, 2016WASHINGTON, D.C.— The American Institute for Medical and Biological Engineering (AIMBE) has announced the pending induction of Xavier Intes, Ph.D., Associate Professor, Biomedical Engineering, Rensselaer Polytechnic Institute, to its College of Fellows. Dr. Intes was nominated, reviewed, and elected by peers and members of the College of Fellows For outstanding contributions to Biophotonics through the development of innovative functional and molecular optical imaging techniques in industry and academia.
 AIMBE
AIMBE
