Jennifer Elisseeff, Ph.D.
AIMBE College of Fellows Class of 2008 For outstanding achievements in tissue engineering and the development and biological analysis of materials for regenerative medicine and clinical translation.
Jennifer Elisseeff elected to National Academy of Sciences
Via Johns Hopkins University | May 5, 2023Three Johns Hopkins researchers elected to National Academy of Sciences
Neuroscientist Amy Bastian, biomedical engineer Jennifer Elisseeff, astrophysicist Alex Szalay among 120 new members
Three Johns Hopkins University researchers—neuroscientist Amy Bastian, biomedical engineer Jennifer Elisseeff, and astrophysicist and computer scientist Alex Szalay—have been elected to the National Academy of Sciences in recognition of their distinguished and continuing achievements in original research… Continue reading.
Organic, Transparent, but Robust- Biomimetic Cornea Implants
Via Advanced Science News | September 3, 2018The human eye is a marvelous organ that owes its performance to a lot of specialized components. The outermost of those, and seemingly simplest, is the cornea. The German word for it, “Hornhaut” (callused skin) already hints at one key function of the cornea – protection of the eye.
However, actual callus, being as intransparent as it is, would not make for a well-functioning eye. In this respect it is not surprising that the cornea also is an important optical element of the eye. Being the first element in the optical path, the cornea is the eye’s main diffractive element. Anybody that suffers from astigmatism, like the author of this text, can confirm the cornea’s importance for good unaided eyesight.
Severe damage to the cornea leads to blindness, with cornea transplantation from a donor being the only cure so far. However, the transplant is often rejected by the recipient’s immune system or suffers from slow mechanical failure. In consequence, medical measures for direct cornea reconstruction are desired.
Qiongyu Guo and Anirudha Singh from John Hopkins University, Jennifer H. Elisseeff form John Hopkins University and the John Hopkins School of Medicine, and their co-workers report successful assembly of collagen into artificial corneal tissue with the help of cyclodextrin… Continue reading.
Jennifer Elisseeff elected to National Academy of Engineering
Via Johns Hopkins University | February 8, 2018Two Johns Hopkins University researchers were awarded one of the highest professional distinctions for engineers: election into the National Academy of Engineering.
The academy announced Wednesday that Jennifer H. Elisseeff, a professor of biomedical engineering; and Charles Meneveau, a professor of mechanical engineering, were among 83 new members, along with 16 foreign members.
According to the academy, becoming a member “honors those who have made outstanding contributions to ‘engineering research, practice, or education, including, where appropriate, significant contributions to the engineering literature’ and to ‘the pioneering of new and developing fields of technology, making major advancements in traditional fields of engineering, or developing/implementing innovative approaches to engineering education.’ ”
Elisseeff, who is also a professor at the Wilmer Eye Institute and directs the Translational Tissue Engineering Center, was chosen for her work in the development and commercial translation of injectable biomaterials for regenerative therapies… Continue reading.
New Joint Lubrication Technique Could Aid Arthritis Treatment
Via Arthritis Research UK | August 20, 2014Scientists in the US have developed a new means of improving the lubrication of arthritic joints by mimicking one of the body’s natural functions.
Researchers at Johns Hopkins University have been able to bind a molecule naturally found in the fluid surrounding healthy joints, making it possible to create surfaces that can deliver long-lasting lubrication at specific spots throughout the body.
Published in the journal Nature Materials, the study took advantage of the natural lubricant properties of the biochemical known as hyaluronic acid (HA), which is found in large quantities in the synovial fluid around the joints.
Utilising HA-binding peptides as a chemical handle, the researchers used a second synthetic molecule called polyethylene glycol to tie HA on to various surfaces, including natural and artificial cartilage.
Tests using tissues and animal subjects demonstrated that the bound HA was not only difficult to wash away, but was also able to reduce friction as successfully as when the tissues were immersed in HA.
The scientists believe this new technique could potentially offer a new way of easing the pain experienced by patients with arthritic joints, or as a method of lubricating artificial joints to keep them moving smoothly.
Currently, the process of injecting HA into painful joints – known as viscosupplementation – is limited by the fact that the body’s natural cleaning processes quickly wash the substance away.
Study leader Dr Jennifer Elisseeff, professor at the Wilmer Eye Institute at Johns Hopkins University, said: "What I like about this concept is that we’re mimicking natural functions that are lost using synthetic materials."
Johns Hopkins Students Tackle Engineering Challenges Around the World
Via The Gazette | January 15, 2014The riverside village of Nazaçu appears on preciously few travel itineraries and barely registers on any map. But in the summer of 2012, Nate Nicholes, a doctoral student in the Whiting School’s Department of Chemical and Biomolecular Engineering, found himself with a group of Johns Hopkins faculty and students cruising down the Brazilian Amazon to this remote portion of the world.
Nazaçu was the group’s second stop, a fishing village of fewer than 100 people that consisted of a church, a school, a single row of homes on stilts, and a community gas-powered mill used to grind cassava tubers into raw flour.
For the villagers, the mill had become both indispensable and a scourge. To grind the cassava, a hard dense root and a staple of the villagers’ diet, mill operators fed the tubers by hand into the machine’s mouth toward a grinding wheel armed with sharp blades. Hand nicks and cuts were commonplace, and some users lost fingers. The mill also produced a blizzard of flying debris known to cause injuries to eyes and face, with anecdotal reports of blindness. All this for a population without direct access to a trauma center.
The villagers wanted a safer machine, but buying a new mill was not an option because of both lack of funds and a reluctance to use a device that needed to be frequently serviced or repaired, as the nearest major town was an hour away by canoe.
Nicholes saw a problem worth solving. In other words, he got just what he came for.
Nicholes’ trip to the Amazon was funded by the Global Engineering Innovation Program, founded in 2011 and hosted by the Johns Hopkins Institute for NanoBioTechnology. The program, seeded by a grant from the Office of the President, annually supports teams of Johns Hopkins students as they investigate and tackle engineering challenges in the developing world.
Jennifer Elisseeff, the program’s director and the Jules Stein Professor of Ophthalmology at the Wilmer Eye Institute, says that the GEI’s design resembles that of the university’s chapter of Engineers Without Borders but is more targeted to graduate students who can dedicate more years to a project. Students form in teams of two to four with a JHU faculty mentor and a mentor at the host site.
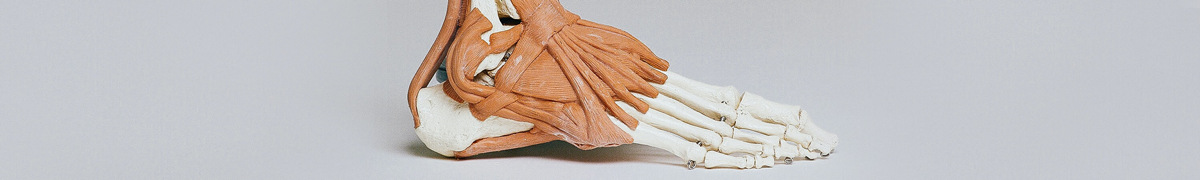
Tissue Engineers Report Knee Cartilage Repair Success With New Biomaterial
Via John Hopkins Medicine | January 14, 2013Proof-of-concept clinical trial in 18 patients shows improved tissue growth
In a small study, researchers reported increased healthy tissue growth after surgical repair of damaged cartilage if they put a “hydrogel” scaffolding into the wound to support and nourish the healing process. The squishy hydrogel material was implanted in 15 patients during standard microfracture surgery, in which tiny holes are punched in a bone near the injured cartilage. The holes stimulate patients’ own specialized stem cells to emerge from bone marrow and grow new cartilage atop the bone.
Results of the study, published in the Jan. 9 issue of Science Translational Medicine, are a proof of concept that paves the way for larger trials of the hydrogel’s safety and effectiveness, the researchers say.
“Our pilot study indicates that the new implant works as well in patients as it does in the lab, so we hope it will become a routine part of care and improve healing,” says Jennifer Elisseeff, Ph.D., Jules Stein Professor of Ophthalmology and director of the Johns Hopkins University School of Medicine’s Translational Tissue Engineering Center (TTEC).
New Composite Material May Restore Damaged Soft Tissue
Via John Hopkins Medicine | August 1, 2012Potential uses include facial reconstruction for soldiers’ blast injuries
Biomedical engineers at Johns Hopkins have developed a new liquid material that in early experiments in rats and humans shows promise in restoring damaged soft tissue relatively safely and durably. The material, a composite of biological and synthetic molecules, is injected under the skin, then “set” using light to form a more solid structure, like using cold to set gelatin in a mold. The researchers say the product one day could be used to reconstruct soldiers’ faces marred by blast injuries.
The Johns Hopkins researchers caution that the material, described in a report in the July 27 issue of Science Translational Medicine, is “promising,” but not yet ready for widespread clinical use.
“Implanted biological materials can mimic the texture of soft tissue, but are usually broken down by the body too fast, while synthetic materials tend to be more permanent but can be rejected by the immune system and typically don’t meld well with surrounding natural tissue,” says Jennifer Elisseeff, Ph.D., Jules Stein Professor of Ophthalmology and director of the Translational Tissue Engineering Center at the Johns Hopkins University School of Medicine. “Our composite material has the best of both worlds, with the biological component enhancing compatibility with the body and the synthetic component contributing to durability.”
Nanoscale Scaffolds and Stem Cells Show Promise in Cartilage Repair
Via John Hopkins Medicine | July 17, 2012Johns Hopkins tissue engineers have used tiny, artificial fiber scaffolds thousands of times smaller than a human hair to help coax stem cells into developing into cartilage, the shock-absorbing lining of elbows and knees that often wears thin from injury or age.
Reporting online June 4 in the Proceedings of the National Academy of Sciences, investigators say they have produced an important component of cartilage in both laboratory and animal models. While the findings are still years away from use in people, the researchers say the results hold promise for devising new techniques to help the millions who endure joint pain.
“Joint pain affects the quality of life of millions of people. Rather than just patching the problem with short-term fixes, like surgical procedures such as microfracture, we’re building a temporary template that mimics the cartilage cell’s natural environment, and taking advantage of nature’s signals to biologically repair cartilage damage,” says Jennifer Elisseeff, Ph.D., Jules Stein Professor of Ophthalmology and director of the Translational Tissue Engineering Center at the Johns Hopkins University School of Medicine.
Building Tissues From Scratch
Via John Hopkins Medicine | February 1, 2011Facing a limited supply of donor tissues and organs, scientists seek to grow their own using stem cells and biodegradable materials.
Cornea transplantation is the most common transplant procedure. In the United States alone, surgeons perform 40,000 of the operations each year. Corneal tissue, however, is in tight supply in this country, and worldwide there is a dire shortage. But what if medical labs could manufacture artificial corneas from components that are easier to come by?
That project is just one of several under way at the recently established Johns Hopkins Translational Tissue Engineering Center, which draws faculty from the Department of Biomedical Engineering and Whiting School of Engineering and is housed in new lab facilities in the school of medicine’s Smith Building…
…The concept of tissue engineering is not new, notes Jennifer Elisseeff, an associate professor of biomedical engineering and director of the Cell and Tissue Engineering Program. Scientists have been working in the field (sometimes called regenerative medicine) for two decades. “But the early plans fizzled,” says Elisseeff. “The primary piece of what was missing before was a practical approach. Pie-in-the-sky promises were made without an appreciation for the complexity in biology and development of these technologies.”
 AIMBE
AIMBE
