James J. Hickman, Ph.D.
AIMBE College of Fellows Class of 2004 For leadership in applying surface modification and analysis to elucidate and control tissue/biomaterials interactions for advanced diagnostic and therapeutic applications.
New System Mimics Human Testing of Therapies for Neuromuscular Junction Diseases Like ALS
Via ALS News Today | May 1, 2018New technology that tests therapies designed for disorders of the neuromuscular junction, such as amyotrophic lateral sclerosis (ALS), closely mimics the human condition and offers a new method of drug testing, according to a report.
The paper, “Stem cell derived phenotypic human neuromuscular junction model for dose response evaluation of therapeutics,” was written by Hesperos Chief Scientific Officer James Hickman, PhD, funded by the National Institutes of Health, and published in the journal Biomaterials.
Hickman is a professor of chemistry, biomolecular science, and electrical engineering at the Hybrid Systems Laboratory at the University of Central Florida.
The new technology is licensed to Hesperos, and is part of the company’s human-on-a-chip program, which re-creates specific human systems in the laboratory for the purpose of toxicology testing and evaluating the effectiveness of new therapies. The new system is available as a fee-for-service assay… Continue reading.
Drs. Hickman & Shuler of Hesperos Awarded 2015 Lush Prize
Via Hesperosinc. | December 1, 2015ORLANDO, Fla. — Hesperos Inc., utilizing technology developed by UCF and Cornell University scientists to enable a more accurate way to test pharmaceuticals without using animal subjects, has been awarded a major international prize.
This innovative technology, known as Body-on-a-Chip or Human-on-a-Chip, was recently awarded the 2015 Lush Prize for Science over 11 finalists from Japan, Switzerland, Germany, South Korea, Australia, the U.K. and the U.S.
Lush, the international cosmetics manufacturer with shops in 49 countries, has awarded the Lush Prize since 2012 in five categories. The 2015 Lush Science award includes a share of $380,000 in prize money.
UCF researcher Dr. James J. Hickman, Professor of Chemistry, Biomolecular Science and Electrical Engineering at the UCF NanoScience Technology Center, partnered with Dr. Michael Shuler at Cornell University to develop functional Body-on-a-Chip systems that are free of animal cells and animal sera.
Hickman and Shuler are utilizing Hesperos, a startup biotech research and development company, to commercialize the technology. Dr. Shuler is President and CEO and Dr. Hickman is Chief Scientist at Hesperos.
Body-on-a-Chip systems work with tissues derived from human cell sources to simulate human metabolism and function, including toxic side effects as well as efficacy from pharmaceutical drug candidates.
“Body-on-a-Chip systems can play a significant role in determining the efficacy and toxicity of new pharmaceuticals without the use of animals,” Dr. Shuler explained.
Dr. Hickman and Shuler’s team is researching ways to improve pharmaceutical testing. Aside from the ethical considerations of using live animal subjects to test potentially life-saving drugs, animal testing is woefully inaccurate.
“For every 50 drugs that are determined to be safe for animals, only one proves safe in humans,” Dr. Hickman said.
A First: Brain Support Cells from Umbilical Cord Stem Cells
Via UCF Office of Research & Commercialization | May 17, 2012For the first time ever, stem cells from umbilical cords have been converted into other types of cells, which may eventually lead to new treatment options for spinal cord injuries and multiple sclerosis, among other nervous system diseases.
This is the first time this has been done with non-embryonic stem cells,” says James Hickman, a University of Central Florida bioengineer and leader of the research group, whose accomplishment is described in the Jan. 18 issue of the journal ACS Chemical Neuroscience.
“We’re very excited about where this could lead because it overcomes many of the obstacles present with embryonic stem cells.
A First: UCF Lab Creates Cells Used by Brain to Control Muscle Cells
Via UCF Office of Research & Commercialization | November 22, 2011University of Central Florida researchers, for the first time, have used stem cells to grow neuromuscular junctions between human muscle cells and human spinal cord cells, the key connectors used by the brain to communicate and control muscles in the body.
The success at UCF is a critical step in developing “human-on-a-chip” systems. The systems are models that recreate how organs or a series of organs function in the body. Their use could accelerate medical research and drug testing, potentially delivering life-saving breakthroughs much more quickly than the typical 10-year trajectory most drugs take now to get through animal and patient trials.
“These types of systems have to be developed if you ever want to get to a human-on-a-chip that recreates human function,” said James Hickman, a UCF bioengineer who led the breakthrough research. “It’s taken many trials over a number of years to get this to occur using human derived stem cells.”
Hickman’s work, funded through the National Institute of Neurological Disorders and Stroke (NINDS) at the National Institutes of Health, is described in the December issue of Biomaterials. (http://www.sciencedirect.com/science/article/pii/S0142961211010556)
Hickman is excited about the future of his research because several federal agencies recently launched an ambitious plan to jump-start research in “human-on-a-chip” models by making available at least $140 million in grant funding.
$1.9 Million Grant To Help UCF Find Multiple Sclerosis ‘Nerve-Ana’
Via UCF Newsroom | May 10, 2010A National Institutes of Health grant will help University of Central Florida researchers explore new ways to potentially reverse the damage caused by multiple sclerosis and other neurological disorders.
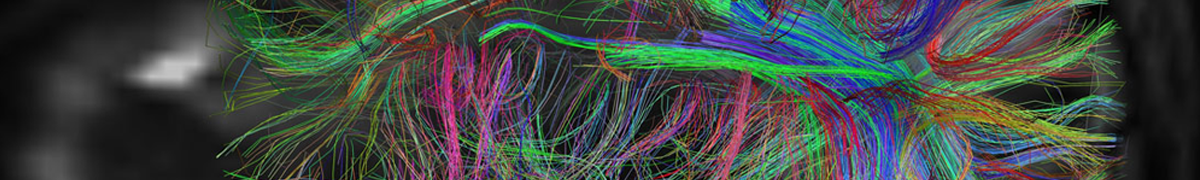
Stephen Lambert, an associate professor in the College of Medicine and a member of UCF’s Hybrid Systems Laboratory, has received $428,000, the first installment of a four-year, $1.9 million project. His team will study the breakdown of myelin, a substance that coats and protects nerves inside the brain and spinal cord, enabling electrical signals to reach distant nerve cells and muscles.
About 400,000 Americans and about 2.5 million people worldwide suffer from MS, according to the National Multiple Sclerosis Society. The drugs that are available now focus mainly on controlling the inflammatory nature of the diseases to limit the development of neuronal damage. They do not reverse the damage caused by the diseases.
“The process of myelination is extremely complex. By reproducing these complex phenomena in our laboratories, we can learn more about what causes debilitating diseases that affect so many people around the world,” Lambert said. “We hope our research will ultimately lead to new drugs that reverse the damage caused by these diseases and help patients lead longer, healthier lives.”
Most of the research will take place in the Hybrid Systems Lab in UCF’s NanoScience Technology Center. At the center, a research team led by UCF bioengineer James Hickman showed for the first time last year that specialized myelin coating could be produced in the lab environment without the use of any type of growth serum.
UCF Alzheimer’s Discovery Could Lead To Long-Sought Preventive Treatment
Via UCF Newsroom | January 8, 2010Despite a massive global research effort, many basics of Alzheimer’s disease onset remain elusive. This has hampered development of treatments effective during the earliest stages of the disease, when prevention is most likely.
But a new discovery by University of Central Florida researchers has revealed a previously unknown mechanism that may drive the early brain function deterioration of Alzheimer’s victims, thus opening a new exploratory path in the quest for an Alzheimer’s cure.
The research, which will be published Friday, Jan. 8, in the peer-reviewed science and medicine journal PLoS ONE, also demonstrates how the unique application of an existing cell research technique could accelerate the discovery of treatments to exploit the new findings.
Researchers have known for years that a substance called amyloid-beta gums up brain cells when it becomes too concentrated, because it forms damaging deposits on the cells known as plaques. These prevent normal electrical signal generation in the cells, eventually killing them. That drives the memory loss and other problems that plague Alzheimer’s sufferers.
Most Alzheimer’s studies have focused on brain cells already damaged by amyloid-beta or the effects of high concentration of amyloid-beta. The University of Central Florida team, led by James Hickman, head of the UCF NanoScience Technology Center’s Hybrid Systems Laboratory, instead explored impacts of very low amyloid-beta concentrations on healthy cells in an effort to mimic the earlier stages of Alzheimer’s. The results were shocking.
 AIMBE
AIMBE
