Gordana Vunjak-Novakovic, Ph.D.
AIMBE College of Fellows Class of 2000
Tiny killers: How autoantibodies attack the heart in lupus patients
Via EurekAlert | August 20, 2024Columbia team engineers a model of the human heart tissue that demonstrates how autoantibodies directly affect heart disease in lupus patients
Cardiovascular disease is the leading cause of death in patients suffering from lupus, an autoimmune disease in which our immune system attacks our own tissues and organs, the heart, blood, lung, joints, brain, and skin. Lupus myocarditis–inflammation of the heart muscle– can be very serious because the inflammation alters the regularity of the rhythm and strength of the heartbeat. However, the mechanisms underlying this complex disease are poorly understood and difficult to study.
A long-standing question about lupus is why some patients develop myocarditis while others remain unaffected. And why the clinical manifestations of affected patients range so dramatically, from no symptoms at all to severe heart failure. Lupus is characterized by a large number of autoantibodies, immune proteins that mistakenly target a person’s own tissues or organs, with different specificities for various molecules. Like our genes, they may explain why different individuals experience different symptoms… Continue reading.
A lung-mimicking sealant helps repair surgical leaks
Via Advanced Science News | March 12, 2024A superior surgical sealant mimics the structural and mechanical properties of lung tissue to repair air leaks after surgery.
A new sealant meant to mimic lung tissue has been shown to rapidly cork air leaks following surgery. Moreover, the protein-like molecules within the sealant were found to potentially help with wound repair.
“Our lung-mimetic sealant is designed with a structure similar to that of the healthy lung, allowing the sealant to deform in a similar way as the breathing lung,” explained Meghan Pinezich, researcher at Columbia University in the US, and first author on the study, in an email… Continue reading.
Tissue chip developments: what’s the 411?
Via News Wise | October 4, 2022Tissue chips—tiny mimics of human organs, just millimeters in size—represent an alternative to animal models as a way to study disease or evaluate drugs. However, a major limitation of tissue chips is that they do not faithfully imitate tissue interactions, so it’s impossible to know how a treatment for liver disease, for example, might affect another organ, like the heart.
To improve this technology, NIBIB-funded researchers have developed an interlinked tissue chip system that can model four mature organs in their perspective environments simultaneously. These multi-organ tissue chips, which could be personalized to model individual patients, may represent a new way to evaluate the systemic effects of novel drugs… Continue reading.
Plug-and-play organ-on-a-chip can be customized to the patient
Via Science Daily | April 27, 2022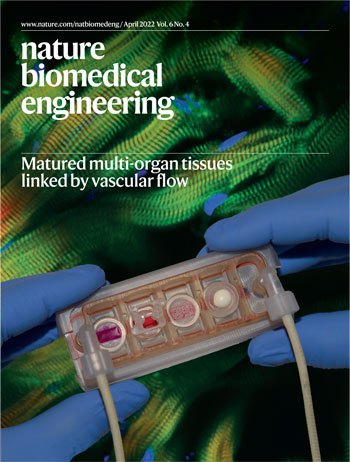 Engineered tissues have become a critical component for modeling diseases and testing the efficacy and safety of drugs in a human context. A major challenge for researchers has been how to model body functions and systemic diseases with multiple engineered tissues that can physiologically communicate — just like they do in the body. However, it is essential to provide each engineered tissue with its own environment so that the specific tissue phenotypes can be maintained for weeks to months, as required for biological and biomedical studies. Making the challenge even more complex is the necessity of linking the tissue modules together to facilitate their physiological communication, which is required for modeling conditions that involve more than one organ system, without sacrificing the individual engineered tissue environments.
Engineered tissues have become a critical component for modeling diseases and testing the efficacy and safety of drugs in a human context. A major challenge for researchers has been how to model body functions and systemic diseases with multiple engineered tissues that can physiologically communicate — just like they do in the body. However, it is essential to provide each engineered tissue with its own environment so that the specific tissue phenotypes can be maintained for weeks to months, as required for biological and biomedical studies. Making the challenge even more complex is the necessity of linking the tissue modules together to facilitate their physiological communication, which is required for modeling conditions that involve more than one organ system, without sacrificing the individual engineered tissue environments.
Novel plug-and-play multi-organ chip, customized to the patient
Up to now, no one has been able to meet both conditions. Today, a team of researchers from Columbia Engineering and Columbia University Irving Medical Center reports that they have developed a model of human physiology in the form of a multi-organ chip consisting of engineered human heart, bone, liver, and skin that are linked by vascular flow with circulating immune cells, to allow recapitulation of interdependent organ functions. The researchers have essentially created a plug-and-play multi-organ chip, which is the size of a microscope slide, that can be customized to the patient. Because disease progression and responses to treatment vary greatly from one person to another, such a chip will eventually enable personalized optimization of therapy for each patient. The study is the cover story of the April 2022 issue of Nature Biomedical Engineering… Continue reading.
Gordana Vunjak-Novakovic Receives AIMBE’s Highest Award
Via AIMBE | March 22, 2021 AIMBE is honored to recognize Gordana Vunjak-Novakovic with its Pierre Galletti Award, the Institute’s highest accolade. Including years of contributions to AIMBE and the BME community, Vunjak-Novakovic is recognized for impactful innovations in technologies to generate, understand and utilize functional human tissues, especially in regenerative engineering, studies of development and disease, while inspiring the next generation of practitioners. This award is presented to an individual in recognition of his/her contributions to public awareness of medical and biological engineering, and to the advancement of biomedical public policy in science, engineering, and education. Register for the AIMBE Annual Meeting and watch Dr. Vunjak-Novakovic’s acceptance remarks on March 26 at 4:10 p.m. ET. Six AIMBE Professional Impact Awardees will also be announced. Join and support your colleagues for their distinguished achievements.
AIMBE is honored to recognize Gordana Vunjak-Novakovic with its Pierre Galletti Award, the Institute’s highest accolade. Including years of contributions to AIMBE and the BME community, Vunjak-Novakovic is recognized for impactful innovations in technologies to generate, understand and utilize functional human tissues, especially in regenerative engineering, studies of development and disease, while inspiring the next generation of practitioners. This award is presented to an individual in recognition of his/her contributions to public awareness of medical and biological engineering, and to the advancement of biomedical public policy in science, engineering, and education. Register for the AIMBE Annual Meeting and watch Dr. Vunjak-Novakovic’s acceptance remarks on March 26 at 4:10 p.m. ET. Six AIMBE Professional Impact Awardees will also be announced. Join and support your colleagues for their distinguished achievements.
Researchers Use Lab-grown Tissue Grafts for Personalized Joint Replacement
Via Columbia Engineering | October 14, 2020The temporomandibular joint (TMJ), which forms the back portion of the lower jaw and connects your jaw to your skull, is an anatomically complex and highly loaded structure consisting of cartilage and bone. About 10 million people in the United States alone suffer from TMJ dysfunction due to birth defects, trauma, or disease. Current treatments range from steroid injections that provide only a temporary pain relief, to surgical reconstructions using either prosthetic devices or donor tissue, and often fail to provide long-lasting repair. Researchers have sought a better way to treat TMJ, including investigating biological TMJ grafts grown in the lab that could integrate with the native tissues, remodel the joint over time, and provide life-long function for the patient.
A multidisciplinary team from Columbia Engineering, Columbia’s College of Dental Medicine and Department of Medicine, Louisiana State University, LaCell LLC, and Obatala Sciences has now bioengineered living cartilage-bone TMJ grafts, precisely matched to the recipient, both biologically and anatomically. Their most recent study, published today in Science Translational Medicine, builds upon a long series of their previous developments that began in 2005 on bioengineering functional cartilage and bone for regenerative medicine and tissue models of disease… Continue reading.
Connecting donated human lungs to pigs repaired damage to the organs, scientists report
Via Stat News | July 13, 2020For people who need a lung transplant, the wait is often prolonged by the frustrating fact that most donor organs have to be discarded: Only 20% of donated lungs meet medical criteria for transplantation, translating into far fewer organs than people on waiting lists. Now, a team of researchers has shown they might be able to salvage more of these lungs by borrowing a pig’s circulatory system.
Delicate lungs recovered from donors are typically connected to perfusion machines that keep oxygen and nutrients flowing to maintain viability, but that works for only about six hours, not long enough for often-injured lung tissue to recover before the organ fails.
Matthew Bacchetta of Vanderbilt University and Gordana Vunjak-Novakovic of Columbia University led a team that extended the current six-hour window for lungs outside the body to 24 hours. As they reported Monday in Nature Medicine, they did it by connecting each of five human lungs declined as too damaged for transplantation to a pig, sharing the animal’s liver, kidney, and other functions… Continue reading.
New approach shows regeneration of severely damaged lungs
Via EurekAlert | May 7, 2019Lung transplantation, the only lifesaving therapy for an increasing population of patients with end-stage lung disease, is severely limited by the number of available donor organs. Currently, up to 80 percent of donor lungs are rejected for serious but potentially reversible injuries. Since the beginning of transplantation in the 1960s, clinicians and scientists have been trying to address the critical shortage of donor organs.
Now, a multidisciplinary team from Columbia Engineering and Vanderbilt University has–for the first time–demonstrated in a clinically relevant model that severely damaged lungs can be regenerated to meet transplantation criteria. In a study published today on Nature Communications ‘ website, the researchers describe the cross-circulation platform that maintained the viability and function of the donor lung and the stability of the recipient for 36 to 56 hours. As Brandon Guenthart, a lead author of the study, explains, “to support lung recovery and to demonstrate cellular regeneration, we had to pursue a radically different approach and develop more minimally invasive diagnostics.” Current methodologies of lung support are limited to only 6 to 8 hours, a time that is too short for therapeutic interventions that could regenerate the injured lung and improve its function… Continue reading.
Gordana Vunjak-Novakovic Elected to American Academy of Arts & Sciences
Via Columbia University | April 18, 2019Biomedical engineer Gordana Vunjak-Novakovic, PhD, University Professor, has been elected to the American Academy of Arts & Sciences.
In her laboratory at Columbia University Irving Medical Center, Vunjak-Novakovic creates new ways to engineer human tissues that could repair damaged organs, help scientists study development and disease, and provide faster methods for testing new drugs.
Her research has potential to develop new materials and techniques to grow bone grafts for facial reconstruction, create heart patches that could repair damage sustained after a heart attack, and improve the way lungs are recovered for transplantation, possibly expanding the pool of available donor lungs. The lab is also designing “organs on a chip”–miniature tissues and organs that mimic human physiology–to test new drugs and personalize patient treatment… Continue reading.
New Cell Therapy Aids Heart Recovery—Without Implanting Cells
Via Columbia University | April 23, 2018Heart disease is a major global health problem—myocardial infarction annually affects more than one million people in the U.S. alone, and there is still no effective treatment. The adult human heart cannot regenerate itself after injury, and the death of cardiac muscle cells, known as cardiomyocytes, irreversibly weakens the heart and limits its ability to pump blood.
Researchers have turned their focus to stem cell transplantation for cardiomyocyte replacement and recovery of heart function, but studies have shown that implanted stem cells have difficulty surviving and differentiating into cardiomyocytes to repair the damaged muscle. When stem cells were differentiated into cardiomyocytes before implantation, heart function improved, but with a complication: the implanted cardiomyocytes did not contract synchronously with the heart, thus causing potentially lethal arrhythmias (abnormal heart rhythm).
A team of Columbia University investigators, led by Biomedical Engineering Professor Gordana Vunjak-Novakovic, has designed a creative new approach to help injured hearts regenerate by applying extracellular vesicles secreted by cardiomyocytes rather than implanting the cells… Continue reading.
Adult-like Human Heart Muscle Grown from Patient-specific Stem Cells
Via Columbia University | April 4, 2018
Photo shows the muscle (dark red, cardiac Troponin T stain) and T-tubules (green invaginations going into the muscle, like thin lines – a hallmark of adult human myocardium never shown before for an engineered heart tissue). —Image credit: Gordana Vunjak-Novakovic/Columbia Engineering
Growing human cardiac tissue that behaves like native heart muscle would be transformative for biomedical research, enabling researchers to study human physiology and model heart diseases under fully controlled conditions. While today scientists can grow many tissues, including the heart muscle, from stem cells taken from a small blood sample of any of us, current bioengineered tissues fail to show some of the most critical hallmarks of adult human heart function. Researchers have not been able to build a cultured heart muscle mature enough to be useful for medical research—until now.
Investigators at Columbia Engineering have developed a radically new approach to growing in the lab adult-like human heart muscle from blood-derived human induced pluripotent stem cells (iPSCs), over only four weeks of bioreactor cultivation. They essentially compressed the timeframe for development, which normally takes nine months, into a faster and more complete transition to cardiac maturity than any other team has been able to achieve. Their methodology is to form human cardiac tissues from early-stage iPSC-derived cardiomyocytes, soon after the initiation of spontaneous contractions, by subjecting the cells encapsulated in hydrogel to increasingly intense physical conditioning. Their findings are published today in Nature.
“Many of the ongoing efforts—including those from our lab—have been biomimetic in nature, trying to recapitulate the known events present during native development,” says the study’s senior author Gordana Vunjak-Novakovic, University Professor, The Mikati Foundation Professor at Columbia Engineering, and professor of medicine at Columbia University Vagelos College of Physicians and Surgeons. “Because these efforts have been limited in how much maturation can be achieved, we decided to try something totally new: to explore the concept of accelerated development. It took a lot of creative thinking and clever engineering by the whole team across both campuses of Columbia University to develop the model we now have, a highly matured, patient-specific heart muscle that can be used for studies of heart development, physiology, disease, and responses to drugs.”… Continue reading.
This Radical New Method Regenerates Failing Lungs With Blood Vessels Intact
Via Singularity Hub | September 20, 2017Save for the occasional burning pain that accompanies a run, most people don’t pay much attention to the two-leafed organ puffing away in our chests.
But lungs are feats of engineering wonder: with over 40 types of cells embedded in a delicate but supple matrix, they continuously pump oxygen into the bloodstream over an area the size of a tennis field. Their exquisite tree-like structure optimizes gas exchange efficiency; unfortunately, it also makes engineering healthy replacement lungs a near-impossible task.
Rather than building lungs from scratch, scientists take a “replace and refresh approach”: they take a diseased lung, flush out its sickly, inflamed cells and reseed the empty matrix with healthy ones.
It’s an intricate procedure—nevertheless, the delicate branches of blood vessels are often completely destroyed during the process. Without blood to deliver nutrients and molecules to the newly seeded cells, the graft fails.
What if, thought Dr. Gordana Vunjak-Novakovic at Columbia University, rather than removing all cells from a donor lung, we gently clean out only the diseased cells in the airway without touching blood circulation?
This week, Vunjak-Novakovic’s team published a “radically new approach” to bioengineering lungs: making scaffolds with blood vessels intact… Continue reading.
Tissue Engineer Gordana Vunjak-Novakovic Earns Columbia’s Highest Academic Honor
Via Columbia | April 13, 2017Gordana Vunjak-Novakovic, a pioneer in the engineering of functional human tissue for use in regenerative medicine, has been appointed to the rank of University Professor, Columbia University’s highest academic honor. Her research has led to the development of novel biomaterials and scaffold architectures for growing bone grafts for facial reconstruction, the creation of electromechanically functional cardiac tissue, the recovery of donor lungs for transplant, the design and use of “organs on a chip” for precision medicine, and other innovations. She is the first professor from Columbia Engineering to receive this honor.
In announcing Vunjak-Novakovic’s appointment on April 13, University President Lee Bollinger highlighted the social impact of her research, her extensive partnerships in academia and industry, her outreach and mentoring of students and young faculty, and her entrepreneurial success as founder of three public-spirited biotechnology companies.
“The discoveries emerging from her laboratory have led to new approaches for treating injuries and complex diseases and also have supported the development and evaluation of therapeutic drugs,” Bollinger wrote. “Professor Vunjak-Novakovic has displayed a special talent for crossing disciplinary boundaries in service of scientific discovery, an inclination that will serve her well as University Professor.”
Vunjak-Novakovic, currently the Mikati Foundation Professor of Biomedical Engineering, Professor of Medical Sciences, and director of Columbia’s Laboratory for Stem Cells and Tissue Engineering, spread that praise to her colleagues and students.
Q&A: Gordana Vunjak-Novakovic
Via Columbia | July 27, 2015Gordana Vunjak-Novakovic’s research is making it possible to engineer human bone and build parts of the heart and lung. An innovative researcher, Vunjak-Novakovic also has launched two start-ups in the course of two years: EpiBone, a bone reconstruction company that allows patients to “grow their own bone,” and TARA Biosystems, which is developing a platform to provide physiologically relevant human heart tissue models for drug testing.
For more than 20 years, Vunjak-Novakovic has made tremendous headway in the emerging field of tissue engineering and regenerative medicine, earning numerous honors along the way. She is a member of the National Academy of Engineering and the Institute of Medicine of the National Academies and a founding fellow of the Tissue Engineering and Regenerative Medicine Society; most recently, she was elected to the American Association for the Advancement of Science (AAAS) and the National Academy of Inventors.
Over winter break, fresh from a trip to Miami to visit her son, Vunjak-Novakovic gave Columbia Engineering magazine access to her lab and discussed the start of her tissue engineering career, her love of music, and works of art that she returns to time and again.
Professors Vunjak-Novakovic Elected to the National Academy of Inventors
Via Columbia | December 17, 2014Of the honor, Vunjak-Novakovic says, ”This really means a lot to me. All our work in the lab is done with eventual applications in mind, and we are actively commercializing some of our technologies. I am happy about being recognized as an inventor, and to be in such good company.”
Vunjak-Novakovic directs the Laboratory for Stem Cells and Tissue Engineering, which is focused on engineering human tissues for regenerative medicine, stem cell research, and modeling of disease. Extensively published and highly cited, she has over 70 licensed, issued, and pending patents, has founded two biotech companies, and is a frequent advisor to government and industry. Among her many recognitions, Vunjak-Novakovic is a fellow of the American Institute for Medical and Biological Engineering, a member of the New York Academy of Science, Academia Europaea, Serbian Academy of Sciences and Arts, and the Women in Technology International Hall of Fame. In 2012, she was elected to the National Academy of Engineering, becoming the first female professor at Columbia University to ever receive this distinction, and, in 2014, elected to the Institute of Medicine of the National Academies.
Prof. Vunjak-Novakovic Named AAAS Fellow
Via Columbia | December 9, 2014Gordana Vunjak-Novakovic, The Mikati Foundation Professor of Biomedical Engineering and a professor of medical sciences (in Medicine) at Columbia University, has been named a fellow of the American Association for the Advancement of Science (AAAS) “for distinguishing contributions to the field of tissue engineering, particularly by developing functional human tissues for regenerative medicine, stem cell research, and modeling of disease.” She joins three P&S faculty members who are among 401 new fellows honored for their contributions to innovation, education, and scientific leadership. She and her co-fellows will be honored in February at the AAAS Fellows Forum during the 2015 AAAS annual meeting in San Jose, CA.
With Wires and Electrodes, Tara Bio Builds a Heart on a Chip
Via Xconomy | November 12, 2014It’s been pretty clear for some time that there’s a big need to improve the efficiency of drug R&D. By industry’s count, drugs cost over $1 billion to develop, and most of them fail. A big reason why is the preclinical studies in petri dishes and animals don’t accurately predict how a drug will behave in humans.
That problem has prompted a slew of companies to innovate new ways to test drugs in a more human-representative fashion, and perhaps even change how preclinical testing is done. The latest to come along is Tara Biosystems, a New York-based Columbia University spinout whose founders say they’ve found a novel, stem-cell based approach that can simulate how a human heart would react to a drug.
Tara recently started up with the help of seed funding from New York-based Harris & Harris Group (NASDAQ: TINY), a publicly-traded venture firm that invests in early-stage companies. Misti Ushio, a managing director and executive VP of Harris & Harris, is leading the company, which is being incubated within the firm.
Regulatory filings show that Harris & Harris has invested around $300,000 in Tara. Ushio says the seed funding gives the company about a year’s worth of runway to prove itself—to validate its technology, convince pharmaceutical companies of its worth, and essentially earn an additional investment, like a full-fledged Series A round.
Tara is based on the work of two researchers: Columbia professor Gordana Vunjak-Novakovic and University of Toronto professor Milica Radisic. They met several years ago at Bob Langer’s lab at MIT and have since worked together to turn stem cells into mature heart tissue that can be tested as if it were an adult heart.
At the core of Tara’s technology are what the founders call “biowire.” Two parallel polymer wires are attached to the wells of a 96-well microplate (pictured above), a common piece of research equipment; the wells function as small test tubes.
The idea is that a researcher would put stem cells into the wells, and then mature them with the help of electrical stimulation. The stem cells grab on to the polymer wires and grow across them as they mature, eventually forming what amounts to tiny micro-hearts, with all of the different cell types that constitute adult heart tissue. Those tiny hearts beat, and pull on the wires when they do. The wires allow for tension, which is important, because by measuring how those wires move, a researcher could determine how the heart contracts, and what, specifically, is causing it to contract in the way it does.
With Wires and Electrodes, Tara Bio Builds a Heart on a Chip
Via Xconomy | November 12, 2014Tara is based on the work of two researchers: Columbia professor Gordana Vunjak-Novakovic and University of Toronto professor Milica Radisic. They met several years ago at Bob Langer’s lab at MIT and have since worked together to turn stem cells into mature heart tissue that can be tested as if it were an adult heart.
At the core of Tara’s technology are what the founders call “biowire.” Two parallel polymer wires are attached to the wells of a 96-well microplate (pictured above), a common piece of research equipment; the wells function as small test tubes.
The idea is that a researcher would put stem cells into the wells, and then mature them with the help of electrical stimulation. The stem cells grab on to the polymer wires and grow across them as they mature, eventually forming what amounts to tiny micro-hearts, with all of the different cell types that constitute adult heart tissue. Those tiny hearts beat, and pull on the wires when they do. The wires allow for tension, which is important, because by measuring how those wires move, a researcher could determine how the heart contracts, and what, specifically, is causing it to contract in the way it does.
The idea is that these measurements, on mature heart tissue, would give pharmaceutical companies a more accurate read on how drugs affect a human heart before they’re tested in people and potentially cause cardiotoxicity, or damage to the heart—a death knell for many drugs, not to mention hazardous for patients.
“People want all the features of the heart in one place, so you can see the interactions and how one thing influences the other,” says Ushio. “And then you can test new medicines to see how that changes.”
Tara envisions researchers using any stem cell type for this process, either grown in their own labs or purchased from a company such as Madison, WI-based Cellular Dynamics (NASDAQ: ICEL).
Professor Gordana Vunjak-Novakovic Elected to the Institute of Medicine
Via Columbia Engineering | October 22, 2014Gordana Vunjak-Novakovic, The Mikati Foundation Professor of Biomedical Engineering and a Professor of Medical Sciences (in Medicine) at Columbia University, has been elected to the elite Institute of Medicine (IOM) of the National Academies. She joins two Columbia University Medical Center (CUMC) faculty members and an adjunct faculty member elected to the IOM’s Class of 2014, one of the highest honors in the fields of medicine and health.
“I was thrilled to hear the news, this is such a great honor,” says Vunjak-Novakovic, who is also the director of the Laboratory for Stem Cells and Tissue Engineering, co-director of the Craniofacial Regeneration Center, and scientific director of Columbia Stem Cell Core. “My lab is diligently working on developing new technologies for regenerating bone, heart, and lung, and for drug testing in human tissue platforms. We are just entering the era of personalized medicine, and this is a most exciting time to be a biomedical engineer. With all the collaborative efforts between the Engineering School and CUMC, we have a great opportunity to advance personalized medicine in a rather unique way.”
Vunjak-Novakovic was elected into the National Academy of Engineering in 2012, becoming the first woman at Columbia to ever earn that prestigious distinction. With her election to the IOM, she becomes the second Columbia Engineering faculty to become a member of these two preeminent medical and scientific organizations in the world, joining her colleague Van C. Mow, Stanley Dicker Professor of Biomedical Engineering and professor of orthopedic engineering.
Prof. Vunjak-Novakovic Wins $6.3M NIH Grant to Design Tissue Chip to Evaluate Drugs
Via Columbia | October 1, 2014The National Institutes of Health (NIH) has just announced major funding for the next three-year phase of its Tissue Chip for Drug Screening program, aimed at improving ways of predicting drug safety and effectiveness, and a team led by Gordana Vunjak-Novakovic, Mikati Foundation Professor of Biomedical Engineering and professor of medical sciences, has been awarded an additional $6.3 million of funding over three years, with $3.5M going to Columbia Engineering. The project consortium includes three of the leading laboratories in the country: Sangeeta Bhatia (MIT), Christopher Chen (Boston University in collaboration with Harvard’s Wyss Institute for Biologically Inspired Engineering), and Karen Hirschi (Yale University).
Today, the estimated cost of bringing a new drug to clinics exceeds $1 billion. Still, some 80 percent of candidate drugs fail in human clinical trials because they are found to be unsafe or ineffective, according to the NIH, despite promising preclinical studies in animal and cell models. The majority of drug recalls in the past 40 years have been due to cardiotoxicity (19% of withdrawals), hepatotoxicity (26% of withdrawals), or unpredicted adverse effects of drug interactions. Drug toxicities that pass through preclinical and clinical studies are particularly highly costly. This situation is largely due to poor predictions of drug responses in the human body by both cell culture and experimental animals, and has motivated the development of tissue chips for drug screening.
Vunjak-Novakovic and her team are developing an integrated heart-liver-vascular model system (nicknamed HeLiVa chip) that mimics the function of the human body and can be used to evaluate therapeutic drugs. The system can also be personalized to model specific genetic and disease states to test drugs for their effectiveness and toxicity in the heart or liver.
“This is a very important program and an exciting collaboration between biology and engineering,” says Vunjak-Novakovic.
Bones, Made to Order
Via Nautilus | August 1, 2013Bones can be broken, made from synthetic materials, or carved from other bones in our body. But grow new bones? That just doesn’t happen. Until now. Scientists at Columbia University have shown they can make bones to order.
“Tissue engineers,” those working to grow new organs, including the heart, from stem cells, have been operating for decades. But creating new bones, given their varied density and shapes, is “more complex,” says Gordana Vunjak-Novakovic at Columbia University’s Department of Biomedical Engineering. In their first experiments, the “bone engineers” started small, with facial bones. Recently, Vunjak-Novakovic and Sidney Eisig, a professor of craniofacial surgery at the Columbia University Medical Center, grew parts of the jawbone located by the ear—the vertical ramus and the condyle—and successfully implanted them in a pig.
Creating new bones would allow doctors to avoid the injurious process of carving them out of other bones in a patient. It would bypass the potential rejection of synthetic bones in some patients. To create new organic bones, the Columbia team seeded stem cells in a scaffolding—a piece of an animal bone stripped of all cellular material and carved in the required shape—and pumped nutrients through the growing bone to deliver them to the cells on the inside. As the new bone gets formed by special cells called osteoblasts, the old scaffolding is dissolved by their counterparts, osteoclasts. The result is a fully viable, live bone. With scaling, the same technology can be used to grow any other bones, including vertebrae. “If it works in the face, it can work in the other parts of the body,” Eisig says.
Exploring the Ultimate Frontier: Science in Space
Via Columbia Engineering | January 9, 2013Gordana Vunjak-Novakovic, Mikati Foundation Professor of Biomedical Engineering and a professor of medical sciences, is one of the first seven members to be selected to the board of directors of the Center for the Advancement of Science in Space (CASIS). She joins an accomplished group of academic and scientific leaders who will help direct CASIS, the nonprofit organization that promotes and manages research on board the International Space Station (ISS) U.S. National Laboratory.
“I am really thrilled and honored to serve as one of the science directors on the CASIS board,” says Vunjak-Novakovic, who is also the director of Columbia Engineering’s Laboratory for Stem Cells and Tissue Engineering. “Our work will be as unique as the International Space Station itself, a ‘laboratory’ that lacks gravity and thus allows us to study the effect of this omnipresent force on all kinds of biological and physical processes. We will be working hand-in-hand with NASA to develop a program for the ISS that will push the limits of science and lead to the development of exciting commercial technologies.”
Vunjak-Novakovic is especially interested in space experiments with proteins, cells, and tissues that cannot be done on Earth, and “can serve,” she says, “as a basis for developing new and curative treatment modalities.”
 AIMBE
AIMBE
