Donald Ingber, M.D., Ph.D.
AIMBE College of Fellows Class of 2011 Major contributions to cell and tissue engineering, as well as angiogenesis and cancer research, systems biology, and nanobiotechnology.
Broad-spectrum coronavirus drug developed through AI-enabled dynamic modeling
Via MedicalXpress | June 12, 2025About 30% of all respiratory tract infections are caused by coronaviruses, leading to widespread illnesses and, in some cases, to epidemic and even pandemic outbreaks, as we experienced with the COVID-19 pandemic. Despite the development of groundbreaking technology that enables the design of prophylactic vaccines, access to those vaccines is not equal across the globe, especially in low-resource countries, and also other hesitations prevent their adoption.
In addition, coronavirus variants are emerging that can have higher infectivity and resistance to existing vaccines and antiviral treatments. Therefore, fast-acting antiviral drugs with broad activity against multiple respiratory coronaviruses and the ability to be rapidly distributed as oral treatments are urgently needed… Continue reading.
Amazing Alzheimer’s drug could stop time inside emergency medical patients
Via StudyFinds | August 22, 2024In the race against time that often defines emergency medicine, scientists have made a breakthrough that sounds like science fiction: they’ve found a way to slow down life itself. Researchers at Harvard University’s Wyss Institute for Biologically Inspired Engineering have discovered that a common Alzheimer’s drug can send the body into a state of “suspended animation” — essentially stopping time inside of critically ill patients!
Specifically, researchers found that donepezil (DNP) can induce a hibernation-like state in animals that don’t naturally hibernate. The finding could potentially transform how we handle medical emergencies, extending the crucial “Golden Hour” during which lifesaving treatment is most effective… Continue reading.
Donald E. Ingber elected to the National Academy of Engineering
Via Harvard University | February 10, 2021Honor is among the highest distinctions to be accorded in the field of engineering
Francis J. Doyle III, Dean of the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) and Donald Ingber, Professor of Bioengineering at SEAS, have been elected to the National Academy of Engineering (NAE).
Doyle and Ingber are among 106 new members and 23 international members chosen for their contributions to “engineering research, practice, or education” and to “the pioneering of new and developing fields of technology, making major advancements in traditional fields of engineering, or developing/implementing innovative approaches to engineering education… Continue reading.
Wyss Institute’s nasal swab and toehold switch technologies licensed to facilitate SARS-CoV-2 diagnostic efforts
Via Harvard University | October 5, 2020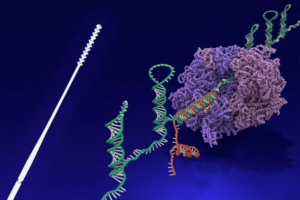
The Wyss Institute for Biologically Inspired Engineering at Harvard University announced today that its nasopharyngeal swab and toehold switch technologies have been licensed to Alabama-based Agile Biodetection, which will use them to develop solutions for unmet diagnostic needs in the detection of the SARS-CoV-2 virus in environmental or clinical settings. The licensing agreement was coordinated by Harvard’s Office of Technology Development (OTD) in accordance with the University’s commitment to the COVID-19 Technology Access Framework.
The Wyss Institute’s nasopharyngeal (nasal) swabs were developed in a multi-institutional and multi-disciplinary group effort led by Wyss Institute Senior Staff Engineer Richard Novak, Ph.D., and the Wyss’ Founding Director Donald Ingber, M.D., Ph.D., as part of the Institute’s collective response to the COVID-19 pandemic. Motivated by the serious shortage of swab devices for the collection of nasopharyngeal samples early in the pandemic, the researchers created a simple and effective device with advantages over other designs. The Wyss swab device is fully injection-molded from a single material, and as such, can be mass manufactured in a one-step process that is faster, less expensive, and routinely used by a broad range of experienced medical device manufacturers worldwide. Conventional nasal swabs that are commonly used in infectious disease diagnostic medicine were designed 50 years ago, and are manufactured in two parts from different materials that then need to be assembled, sterilized and packaged in a multi-step process, which requires considerable time and expense. In successful tests performed by academic collaborators and teaching hospitals, the unique nasal swab design was demonstrated to effectively collect SARS-CoV-2 genetic RNA material from the nostrils of patients and to be more comfortable than existing commercial products… Continue reading.
Repurposing approved drugs for COVID-19 at an accelerated pace
Via Harvard University | June 16, 2020The United States’ Defense Advanced Research Projects Agency (DARPA) has signed an Agreement worth up to $16 million over the next year with the Wyss Institute for Biologically Inspired Engineering at Harvard University to identify and test FDA-approved drugs that could be repurposed to prevent or treat COVID-19. This highly collaborative effort leverages the Institute’s computational drug discovery pipelines and human Organ Chip technologies, and has already found multiple approved compounds that show promise against the SARS-CoV-2 virus that causes COVID-19.
The team, led by Wyss Founding Director Donald Ingber, M.D., Ph.D., is continuing to evaluate many more drugs, and lead compounds are being tested in high-throughput cell-based assays with CoV-2 virus in the lab of Matthew Frieman, Ph.D., Associate Professor of Microbiology and Immunology at the University of Maryland School of Medicine. The most promising drugs are being transferred to the lab of Benjamin tenOever, Ph.D. at the Icahn School of Medicine at Mount Sinai for testing in COVID-19 animal models. Human Organ Chip technology is also being set up in the Frieman and tenOever labs with equipment supplied by Wyss spinout Emulate, Inc., so that they can carry out experiments analyzing the human response to COVID-19 infection in vitro… Continue reading.
Investigating the human intestinal mucus barrier up-close and personal
Via EurekAlert | December 3, 2019We have a mutualistic but complicated relationship with the collection of microbes in our gut known as the intestinal microbiome. This complex community of bacteria breaks down different food components, and releases nutrients such as vitamins and a plethora of other factors that control functions in tissues way beyond the intestinal tract. However, the sheer numbers of microbes also present a threat as they can trigger inflammation, which is thought to be at the root of many intestinal diseases, including inflammatory bowel disease, radiation-induced intestinal injury, and some cancers.
To allow the uptake of beneficial substances from the gut lumen, and at the same time prevent gut microbes from contacting the intestinal epithelial tissue surface, specialized cells called goblet cells continuously produce mucus, the slimy goo-like substance that coats the entire intestinal surface. Mucus thus far has been notoriously difficult to study: its structure quickly disintegrates in surgically removed sections of the gut, the system most often used to study mucus, and no in vitro culture system has been able to reconstitute an in vivo-like mucus layer with the natural structure seen in living intestine outside the human body. Adding to these difficulties, mucus also differs between humans and other species, different sections of the intestinal tract, and even different individuals… Continue reading.
Gut Microbiome Sets Up House in an Intestine Chip
Via Geneng News | May 14, 2019Ordinarily, the microbial flora within the gut are amiable enough. That’s why they qualify as commensal. But when they are taken from their homes and brought to unnatural surroundings, they can quickly wear out their welcome. In fact, within a day, they can overgrow and kill the host human cells in culture dishes. Nonetheless, the gut’s microbes are capable of being good guests—and displaying ordinary host-microbiome behavior—if they are properly accommodated.
To show how hosts can help potentially disagreeable guests remember their etiquette, researchers at Harvard’s Wyss Institute have developed a microfluidic Intestine Chip, that is, an intestine-on-a-chip. It can culture a stable complex human microbiome in direct contact with a vascularized human intestinal epithelium for at least 5 days… Continue reading.
Wyss-developed Antifouling Coating a Boon to Business and Environment
Via Harvard University | August 17, 2017It all began with a bet.
At a conference in Italy in 2013, Nicolas Vogel, then a postdoctoral fellow in Joanna Aizenberg’s lab at the Wyss Institute for Biologically Inspired Engineering at Harvard University and Harvard’s John A. Paulson School of Engineering and Applied Sciences (SEAS), gave a talk about the group’s slippery liquid-infused porous surfaces (SLIPS) coatings, which promised to prevent nearly anything from adhering to structures to which they were applied. In the audience was Ali Miserez, an associate professor of materials science and engineering at Singapore’s Nanyang Technological University (NTU), specializing in biological materials, who approached Vogel after the presentation and said confidently, “I bet mussels will stick to your coatings, because I still have yet to see a surface that they won’t attach to.”
Vogel accepted the challenge, and on returning to Cambridge he sent some SLIPS samples to Miserez, initiating a collaboration whose results are reported in this week’s issue of Science. The study demonstrated that a certain form of SLIPS is indeed essentially mussel-proof, and it shed light on how the coatings thwart mussels’ expert attachment mechanisms… Continue reading.
New robotic exosuit could push the limits of human performance
Via Harvard University | June 2, 2017Wearable technologies for athletes and consumers a growing possibility
By Lindsay Brownell, Wyss Institute Communications
What if you could improve your average running pace from 9:14 minutes/mile to 8:49 minutes/mile without weeks of training?
Researchers at Harvard’s Wyss Institute and the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) at Harvard University have demonstrated that a tethered soft exosuit can reduce the metabolic cost of running on a treadmill by 5.4 percent, bringing those dreams of high performance closer to reality.
“Homo sapiens has evolved to become very good at distance running, but our results show that further improvements to this already extremely efficient system are possible,” says corresponding author Philippe Malcolm, former postdoctoral research fellow at the Wyss Institute and SEAS, and now assistant professor at the University of Nebraska, Omaha, where he continues to collaborate on this work. The study appears today in Science Robotics.
…
“Our work at the Wyss is biologically inspired and, as shown by Conor’s team’s advance, sometimes we learn that a conventional biological view of a mechanism is not really how living systems work; we need to place individual components — in this case, a human hip joint — in context of the living whole. When we do this right, transformative new technologies emerge,” says Wyss Director Donald Ingber, the Judah Folkman Professor of Vascular Biology at Harvard Medical School and the Vascular Biology Program at Boston Children’s Hospital, as well as professor of bioengineering at SEAS. “Studies like this are also a great example of the power of thinking beyond the limitations that nature has handed us and asking, ‘Can we do better?’” … Continue reading.
Printing Metal In Midair
Via Harvard | May 16, 2016“Flat” and “rigid” are terms typically used to describe electronic devices. But the increasing demand for flexible, wearable electronics, sensors, antennas, and biomedical devices has led a research team to innovate an eye-popping way of printing complex metallic architectures as though seemingly suspended in midair.The work was conducted by researchers at Harvard’s Wyss Institute for Biologically Inspired Engineering and the John A. Paulson School of Engineering and Applied Sciences (SEAS) and will be reported online today in the Proceedings of the National Academy of Sciences.
“This sophisticated use of laser technology to enhance 3-D printing capabilities not only inspires new kinds of products, it moves the frontier of solid free-form fabrication into an exciting new realm, demonstrating once again that previously accepted design limitations can be overcome by innovation,” said Wyss Institute Director Donald Ingber, who is also the Judah Folkman Professor of Vascular Biology at Harvard Medical School and the Vascular Biology Program at Boston Children’s Hospital, as well as professor of bioengineering at SEAS.
Donald Ingber elected to American Academy of Arts and Sciences
Via Harvard | April 20, 2016Donald E. Ingber has been elected to Fellow of the American Academy of Arts and Sciences, one of the nation’s oldest and most prestigious honor societies and a leading center for independent policy research.
Ingber, the Judah Folkman Professor of Vascular Biology and Professor of Bioengineering and the founding director and core faculty member of the Wyss Institute for Biologically Inspired Engineering joins a group of some of the world’s most accomplished scholars, scientists, engineers, writers, and artists, as well as civic, business, and philanthropic leaders.
This year’s class includes 175 other new fellows and 37 Foreign Honorary Members. The Academy convenes its leaders from the academic, business, and government sectors to provide policy advice relating to challenges facing the nation and the world.
4D-Printed Structure Changes Shape When Placed In Water
Via Harvard | January 25, 2016A team of scientists at the Wyss Institute for Biologically Inspired Engineering at Harvard University and the Harvard John A. Paulson School of Engineering and Applied Sciences (SEAS) has evolved their microscale 3-D printing technology to the fourth dimension, time.
Inspired by natural structures like plants, which respond and change their form in response to environmental stimuli, the team has unveiled 4D-printed hydrogel composite structures that change shape when immersed in water.
“What’s remarkable about this 4D printing advance made by Jennifer and her team is that it enables the design of almost any arbitrary, transformable shape from a wide range of available materials with different properties and potential applications, truly establishing a new platform for printing self-assembling, dynamic microscale structures that could be applied to a broad range of industrial and medical applications,” said Wyss Institute Director Donald Ingber, the Judah Folkman Professor of Vascular Biology at Harvard Medical School and the vascular biology program at Boston Children’s Hospital and professor of bioengineering at SEAS.
Closer To Detecting When And Why Blood Clots Form
Via Harvard | January 6, 2016Scientists at the Wyss Institute have created a better assay for testing blood’s clotting tendency, which could prove to be a lifesaver for patients with abnormal blood coagulation and platelet function.
As reported in today’s Nature Communications, this bioinspired advance by the Wyss Institute for Biologically Inspired Engineering at Harvard University takes a biophysical approach by subjecting blood to what it would experience inside a patient’s vascular network. It can be used with blood samples or potentially be integrated into patients’ blood-flow lines, offering clinicians the foresight they need to prevent life-threatening blood clotting or internal hemorrhaging.
Led by Donald Ingber, founding director of the Wyss, the team has developed a novel microfluidic device in which blood flows through a lifelike network of small “vessels.” It is here that it’s subjected to true-to-life shear stresses and force gradients of the human vascular network. Using automated pressure sensors and a proprietary algorithm developed by the Wyss team, data acquired from the device is analyzed in real time, precisely predicting when a certain blood sample will obstruct the blood vessel network.
Two faculty elected Fellows of the National Academy of Inventors | Harvard John A. Paulson School of Engineering and Applied Sciences
Via Harvard | December 15, 2015Two faculty members at the John A. Paulson School of Engineering and Applied Sciences (SEAS) – Jennifer Lewis, the Hansjorg Wyss Professor of Biologically Inspired Engineering; and Donald Ingber, Professor of Bioengineering – have been elected fellows of the National Academy of Inventors (NAI).
The NAI chooses fellows from around the world who “have demonstrated a highly prolific spirit of innovation in creating or facilitating outstanding inventions that have made a tangible impact on quality of life, economic development, and the welfare of society.”
Ingber, a cell biologist and bioengineer, is the founding director of the Wyss Institute for Biologically Inspired Engineering at Harvard University and also the Judah Folkman Professor of Vascular Biology at Harvard Medical School and Boston Children’s Hospital. He holds over 140 patents, founded four companies and has pioneered research in mechanobiology, tissue engineering and nanobiotechnology.
Lewis, a materials scientist and 3D printing pioneer, is a core faculty member of the Wyss Institute. She holds more than 30 patents and founded the startup company Voxel8, Inc., to commercialize the first multi-material 3D printing for the fabrication of embedded electronics.
Ingber and Lewis will be inducted on April 15, 2016, at the Fellows Induction Ceremony at the United States Patent and Trademark Office in Alexandria, Virginia.
Human-Gut-On-A-Chip Model Offers Hope For IBD Sufferers
Via Harvard | December 15, 2015It’s estimated that as many as a million Americans suffer from inflammatory bowel diseases (IBD) such as ulcerative colitis and Crohn’s disease, which cause mild to severe symptoms that at best can be managed and at worst lead to life-threatening complications.
While abnormal immune responses are largely responsible for these diseases, issues relating to gut microbiome, intestinal epithelial cells, immune components, and the gut’s rhythmic peristalsis motions can also contribute to and exacerbate symptoms. But until now, scientists have been hard pressed to develop new therapies for treating IBDs because they could not replicate the human gut microenvironment in the laboratory.
On Monday, the Wyss Institute for Biologically Inspired Engineering at Harvard University announced that its team had created a model of human intestinal inflammation and bacterial overgrowth in a human-gut-on-a-chip. The team, co-led by Wyss Institute Founding Director Donald Ingber and core faculty member James Collins, leveraged the institute’s proprietary human-organs-on-chips technology to microengineer the model.
“The discovery of the microbiome and its significance represents a huge paradigm shift in our understanding of human health — there are more microbes living on us and in us than our own cells,” said Ingber, the Judah Folkman Professor of Vascular Biology at Harvard Medical School and the Vascular Biology Program at Boston Children’s Hospital, and professor of bioengineering at the Harvard John A. Paulson School of Engineering and Applied Sciences.
Blood Clot Breakthrough Uses Drug-Device Combo
Via Harvard Gazette | October 28, 2015A new, highly effective drug-device combination for treating life-threatening blood clots in stroke patients is being developed by a team of researchers at Harvard’s Wyss Institute and the University of Massachusetts’ New England Center for Stroke Research.
The study, which will appear in the December issue of the journal Stroke, describes a novel method to quickly dissolve clots that completely obstruct blood vessels in the brain.
The team’s research, which is co-led by Wyss Institute founding director Donald Ingber and University of Massachusetts Medical Professor of Radiology Ajay Wakhloo, combines an injectable clot-busting nanotherapeutic that targets blockages with an intra-arterial device that restores blood flow to obstructed vessels.
The Wyss Institute for Biologically Inspired Engineering at Harvard University had already discovered novel nanotherapeutics for clearing obstructed blood vessels. Its nanotherapeutic is composed of an aggregate of biodegradable nanoparticles coated with a clot-busting drug called tissue plasminogen activator (tPA), which mimics the way blood platelets behave inside our own bodies. When blood vessels narrow, the shear force of blood flow increases at that location to produce a physical cue that causes platelets to stick to the vessel wall. Similarly, the nanotherapeutic reacts to fluid shear force, releasing tPA-coated nanoparticles in these narrowed regions where vessels are partially occluded, binding to the blood clot and dissolving it away.
Wyss Scientists Launch Opsonix With $8M to Fight Blood-Borne Bugs
Via Xconomy | October 8, 2015Donald Ingber is known as a pioneer in the organ-on-a-chip field. But the founding director of Harvard University’s Wyss Institute apparently has some other ideas up his sleeve—like a method of clearing dangerous infections from the blood, a technology that has formed the basis for his latest startup.
Opsonix, a startup spun out of the Wyss in Cambridge, MA, emerged from stealth this morning with $8 million in Series A financing. The cash comes from Baxter Ventures, the venture arm of Baxter International, and Swiss billionaire investor Hansjorg Wyss, the founder of the Wyss.
The work comes from the lab of Ingber, a Harvard professor best known for his pioneering work in the field of organs on chips—a preclinical testing technology meant to increase the odds of a drug’s success when it’s eventually tested in humans. Ingber’s work led to a startup called Emulate, which scored a $12 million Series A last year—a round that Hansjorg Wyss also took part in.
Opsonix is Ingber’s latest startup. He and Wyss staff scientist and biotech veteran Michael Super have come up with what they call “pathogen-capture proteins.” They’re engineered version of opsonins—parts of the innate immune system, the body’s first line of defense. Opsonins bind to pathogens and mark them for destruction by immune cells, which helps the body clear out foreign invaders.
Wyss Institute’s Organs-on-chips Develops into New Company
Via Harvard Gazette | July 29, 2014In order to accelerate the development of new pharmaceuticals, Harvard’s Wyss Institute for Biologically Inspired Engineering announced that its human organs-on-chips technology will be commercialized by a newly formed private company.
The announcement on Monday followed a worldwide license agreement between Harvard’s Office of Technology Development (OTD) and the startup Emulate Inc. The agreement, relating to the use of the institute’s automated human organs-on-chips platform, includes not only pharmaceuticals, but chemical, cosmetic, and personalized medicine products as well.
“This is a big win towards achieving our institute’s mission of transforming medicine and the environment by developing breakthrough technologies and facilitating their translation from the benchtop to the marketplace,” said Wyss Institute Director Donald Ingber, who led the organs-on-chips effort.
Organs-on-chips Evaluate Therapies for Lethal Radiation Exposure
Via Harvard Gazette | August 12, 2013A team at the Wyss Institute for Biologically Inspired Engineering at Harvard University has received a $5.6 million grant from the United States Food and Drug Administration (FDA) to use its organs-on-chips technology to test human physiological responses to radiation and evaluate drugs designed to counter those effects. The effort will also be supported by a team in the vascular biology program at Children’s Hospital Boston.
The multiyear project will investigate whether organs-on-chips — tiny, microfluidic devices that are lined by living human cells and mimic complex organ physiology — can be used instead of animals to evaluate the efficacy and safety of medical treatments for radiation sickness, or acute radiation syndrome (ARS). Animal models often fail to accurately predict human responses, and human subjects cannot be tested with exposure to lethal radiation.
Can We Eliminate Animals from Medical Research?
Via PBS | August 7, 2013Deep in a lab at the Wyss Institute for Biologically Inspired Engineering at Harvard University, Dr. Donald Ingber has reconstructed a human lung. It absorbs oxygen like a normal human lung. It also transmits that oxygen to blood cells flowing beneath. White blood cells flock to foreign bodies that try to infect its tissue, surrounding the invaders and stamping them out. In many ways, it’s indistinguishable from the lungs that rise and fall inside you and me, with one exception. This lung is on a microchip.
On these microchips smaller than your thumb, Ingber, director of the Wyss Institute, has reconstructed the complicated interface between lungs and their capillaries. The core of the device is a tiny tube created by microfabrication—a technique used to make structures on the micrometer scale—which is divided in two by a flexible, porous membrane. Human lung cells line the top of the membrane, and capillary cells coat the underside. Air flows through the upper chamber, and a liquid containing human blood cells runs through the lower chamber. Graduate students apply suction to compartments on the sides, mechanically stretching the membrane and its tissue to simulate the rise and fall of our own chests.
Lung-on-a-Chip Wins Prize
Via Harvard Gazette | February 26, 2013Wyss Institute Founding Director Donald Ingber received the NC3Rs 3Rs Prize from the U.K.’s National Centre for the Replacement, Refinement, and Reduction of Animals in Research (NC3Rs) for his innovative Lung-on-a-Chip — a microdevice lined by human cells that recapitulates complex functions of the living lung.
“We believe that our human breathing Lung-on-a-Chip, and other organ chips we have in development, represent a first wave of exciting new alternative approaches to animal testing that hopefully will change how drug development is carried out in the future,” Ingber said. “This award helps to validate this radical new approach on the global stage, and to strengthen our resolve to work with government agencies and pharmaceutical companies that have been supporting our work to pursue this alternative approach to animal testing.”
Wyss Institute Models a Human Disease in an Organ-on-a-Chip
Via Wyss Institute | November 7, 2012Researchers at the Wyss Institute for Biologically Inspired Engineering at Harvard University have mimicked pulmonary edema in a microchip lined by living human cells, as reported today in the journal Science Translational Medicine. They used this “lung-on-a-chip” to study drug toxicity and identify potential new therapies to prevent this life-threatening condition.
The study offers further proof-of-concept that human “organs-on-chips” hold tremendous potential to replace traditional approaches to drug discovery and development.
“Major pharmaceutical companies spend a lot of time and a huge amount of money on cell cultures and animal testing to develop new drugs,” says Donald Ingber, M.D., Ph.D., founding director of the Wyss Institute and senior author of the study, “but these methods often fail to predict the effects of these agents when they reach humans.”
Building Organs, On One Microchip At A Time
Via NPR | July 27, 2012Bioengineers are developing microchips, about the size of a thumb, that can behave like human organs. Donald Ingber, director of the Wyss Institute for Biologically Inspired Engineering, discusses how the “organ-on-a-chip” works and why the technology could replace the animal model for drug testing.
Harvard’s Wyss Institute Develops Novel Nanotherapeutic that Delivers Clot-Busting Drugs Directly to Obstructed Blood Vessels
Via Wyss Institute | July 5, 2012Researchers at the Wyss Institute for Biologically Inspired Engineering at Harvard University have developed a novel biomimetic strategy that delivers life-saving nanotherapeutics directly to obstructed blood vessels, dissolving blood clots before they cause serious damage or even death. This new approach enables thrombus dissolution while using only a fraction of the drug dose normally required, thereby minimizing bleeding side effects that currently limit widespread use of clot-busting drugs.
The shear-activated nanotherapeutic breaks apart and releases its drug when it encounters regions of vascular narrowing.
The research findings, which were published online today in the journal Science, have significant implications for treating major causes of death, such as heart attack, stroke and pulmonary embolism, that are caused by acute vascular blockage by blood thrombi.
Harvard’s Wyss Institute Creates Living Human Gut-on-a-Chip
Via Wyss Institute | March 27, 2012Researchers at the Wyss Institute for Biologically Inspired Engineering at Harvard University have created a gut-on-a-chip microdevice lined by living human cells that mimics the structure, physiology, and mechanics of the human intestine — even supporting the growth of living microbes within its luminal space. As a more accurate alternative to conventional cell culture and animal models, the microdevice could help researchers gain new insights into intestinal disorders, such as Crohn’s disease and ulcerative colitis, and also evaluate the safety and efficacy of potential treatments. The research findings appear online in the journal Lab on a Chip.
Building on the Wyss Institute’s breakthrough “Organ-on-Chip” technology that uses microfabrication techniques to build living organ mimics, the gut-on-a-chip is a silicon polymer device about the size of a computer memory stick. Wyss Founding Director, Donald Ingber, M.D., Ph.D., led the research team, which included Postdoctoral Fellow, Hyun Jung Kim, Ph.D; Technology Development Fellow, Dan Huh, Ph.D.; and Senior Staff Scientist, Geraldine Hamilton, Ph.D. Ingber is also the Judah Folkman Professor of Vascular Biology at Harvard Medical School and the Vascular Biology Program at Children’s Hospital Boston, and Professor of Bioengineering at Harvard’s School of Engineering and Applied Sciences.
Researchers Develop “Smart” Nanotherapeutics that Deliver Drugs Directly to Pancreas
Via Wyss Institute | January 12, 2012A research collaboration between the Wyss Institute for Biologically Inspired Engineering at Harvard University and Children’s Hospital Boston has developed “smart” injectable nanotherapeutics that can be programmed to selectively deliver drugs to the cells of the pancreas. Although this nanotechnology will need significant additional testing and development before being ready for clinical use, it could potentially improve treatment for Type I diabetes by increasing therapeutic efficacy and reducing side effects.
The approach was found to increase drug efficacy by 200-fold in in vitro studies based on the ability of these nanomaterials to both protect the drug from degradation and concentrate it at key target sites, such as regions of the pancreas that contain the insulin-producing cells. The dramatic increase in efficacy also means that much smaller amounts of drugs would be needed for treatment, opening the possibility of significantly reduced toxic side effects, as well as lower treatment costs.
The research was led by Wyss Institute Founding Director Donald Ingber, M.D., Ph.D., and Kaustabh Ghosh, Ph.D., a former postdoctoral fellow at Children’s Hospital Boston, working within the hospital’s Vascular Biology Program. Their findings appear in the current issue of Nano Letters. Ingber is also the Judah Folkman Professor of Vascular Biology at Harvard Medical School and Children’s Hospital Boston, and Professor of Bioengineering at Harvard’s School of Engineering and Applied Sciences. Ghosh is now an Assistant Professor of Bioengineering at the University of California, Riverside. Wyss Institute Postdoctoral Fellows, Umai Kanapathipillai and Netanel Korin, also contributed to the work, as did Jason McCarthy, Assistant Professor in Radiology at Harvard Medical School and an Assistant in Chemistry at Massachusetts General Hospital.
Wyss Institute Founding Director Donald Ingber Receives 2011 Holst Medal
Via Wyss Institute | December 6, 2011The Wyss Institute for Biologically Inspired Engineering at Harvard University announced today that its Founding Director, Donald Ingber, M.D., Ph.D., has received the 2011 Holst Medal in recognition of his pioneering work exploring the cellular mechanisms that contribute to mechanical control of tissue and organ development and his groundbreaking development of bioinspired technologies, ranging from Organ-on-Chip replacements for animal studies to new engineering approaches for whole organ engineering.
Donald Ingber on the Serendipity of Science
Via PopTech | April 27, 2011It may have been serendipity. While Donald Ingber was enrolled in an undergraduate sculpture course, he was also learning how to culture cells in a biology class, which led him to an unexpected breakthrough in comprehending cellular construction. It’s that same kind of chance that Ingber hopes will infiltrate Harvard University’s Wyss Institute for Biologically Inspired Engineering, where he is the organization’s founding director.
The Wyss Institute launched in 2009 when Harvard received $125 million from Hansjörg Wyss to carry out the Provost’s challenge to envision the future of bioengineering across the entire university.
In his 2010 PopTech talk, Ingber explained that the Institute’s goals were not only to create a new model for technology innovation and collaboration, but also to look to biology to develop new engineering solutions.
Donald Ingber is Uncovering Nature’s Design Principles to Inspire Bioengineering
Via PopTech | October 21, 2010Donald Ingber studies how the natural patterns that have often been dismissed as design flaws might transform the field of bioengineering.
Ingber is the founder and director of the Wyss Institute for Bioinspired Engineering at Harvard. He proposes applying the adaptive and competitive responses of living systems to the fields of engineering in a way that might bring revolutionary advances in engineering, nanotechnology, synthetic biology and computer science.
Ingber’s perspective is based, in part, on his discovery while in an art class in college, that cells are built more like tents than like balloons. This critical insight dramatically changed how he thought about living cells. Hey came to see that they structure themselves in much the same way that inventor Buckminster Fuller dubbed the “tensegrity.” This balance between tension and compression, which Fuller employed to construct his famed geodesic domes, reveals that the design of materials could be viewed as dynamic systems.
Wyss Founding Director Receives Lifetime Achievement Award from the Society of In Vitro Biology
Via Wyss Institute | June 7, 2010Donald E. Ingber, MD, PhD, Founding Director of the Wyss Institute, today received the Lifetime Achievement Award from the Society of In Vitro Biology in recognition of his trailblazing work in advancing the field of in vitro biology. Ingber has developed or applied several technologies — such as microcontact printing, cell magnetometry, laser nanosurgery, and microfluidics — to manipulate cell shape and function.
 AIMBE
AIMBE
