Sina Rabbany, Ph.D.
AIMBE College of Fellows Class of 2012 For his outstanding contribution to the research and understanding of the role that vascular system plays in promoting functional tissue regeneration and for contributions to bioengineering education.
Engineering Customized Blood Vessels to Support Organ Regeneration
Via Hofstra University | October 20, 2020A team of scientists that includes Sina Rabbany, PhD, dean of Hofstra University’s Fred DeMatteis School of Engineering and Applied Science, has pioneered a method for manufacturing functioning human blood vessels that can transport blood, an advancement that could potentially revolutionize the production of human transplantable organs.
“More than 100,000 people on the national transplant waiting list can benefit from a translational approach to repairing damaged organs, but making a functional blood vessel network within complex tissues such as the heart, lung, pancreas, liver, or kidneys has long been a major hurdle” said Dr. Rabbany, professor of engineering and a senior co-author of the study. “The challenge has been in creating a stable vascular network that can undergo self-assembly to allow large organ tissue to repair or rejuvenate itself. This advance now allows us to generate a network of functional blood vessels in a dish… Continue reading.
Molecular Determinants of Nephron Vascular Specialization in the Kidney
Via Hofstra University | January 29, 2020DeMatteis Dean Rabbany Publishes Research in Nature Communications
Research conducted by Dr. Sina Rabbany, dean of the DeMatteis School of Engineering and Applied Science and a team of researchers at Weill Cornell Medicine and University of Texas Southwestern Medical School, was published this month in Nature Communications.
The study, Molecular Determinants of Nephron Vascular Specialization in the Kidney, showed that the cells of blood vessels play a critical role in shaping the growth of other types of cells in the kidney. The study builds on an evolving view that the cells that line blood vessels, called endothelial cells, are the critical architects of tissue and organ development… Continue reading.
Research Conducted by Dean Rabbany and Bioengineering Alum Published in Prestigious Nature Journal
Via Hofstra University | October 17, 2017Research conducted by Dean Sina Rabbany and bioengineering alum Pierre Llanos ’16 on the role that the retina plays in age-related, macular degeneration was recently published the journal Nature Communications.
Their study, Concerted Regulation of Retinal Pigment Epithelium Basement Membrane and Barrier Function by Angiocrine Factors, investigated how endothelial cells regulate the retinal pigment epithelium (RPE) located in the outer layer of the retina. The RPE is an unusual cell that performs many functions essential for our ability to see. It is critical for the survival and function of retinal photoreceptors, which are present in the outer region of the retina. Abnormalities in the RPE are a contributing factor in the development of age-related macular degeneration (AMD), a disease that affects a small area in the center of the retina and blurs the sharp, central vision we use to read and see fine detail. No blood vessels penetrate through the RPE to the outer retina. Instead, the blood supply for the photoreceptors is provided by the choroid… Continue reading.
Dr. Rabbany Continues To Lead SEAS
Via Hofstra | July 7, 2016When Dr. Sina Rabbany was appointed acting dean of SEAS, he had been founding director of the Bioengineering Program at Hofstra and had already established a reputation as a prolific researcher, with more than 60 publications and patents, in the areas of cardiovascular dynamics, biosensors, vascular biology, and tissue engineering/regenerative medicine. His work is also noteworthy for the number of undergraduate researchers he has directed, many of whom have gone on to obtain PhDs/MDs.
Dr. Rabbany joined Hofstra in 1990 as an assistant professor of engineering to create the Hofstra Bioengineering Program, the first on Long Island. Dr. Rabbany has received funding from numerous organizations, including the National Cancer Institute, National Institutes of Health, and the Office of Naval research. He was selected to be a Fellow of the American Institute of Medical & Biological Engineering in 2012.
Since taking on his current post, Dr. Rabbany has seen undergraduate enrollment in SEAS grow from 538 in Fall 2014 to 625 in Fall 2015 and to an estimated 700 in Fall 2016. Graduate enrollment in computer science has also increased from 30 to 50 in the same period. The co-op program, launched in 2015, already boasts approximately 100 companies eager to hire SEAS students for extended full-time paid work experience.
Building Bridges Between the Disciplines
Via Hofstra | April 6, 2016One of the essentials of good engineering design is its integrity, its wholeness. It must conform to a plan, and serve a purpose that harmonizes with the natural world. A great bridge, such as the Golden Gate in San Francisco or the Verrazano Narrows in New York, seems almost an inevitable extension of its environment. It does, of course, fulfill the utilitarian purpose of carrying automobile traffic from one land mass to another, but it also has the power to move an observer to pause and admire its beauty and marvel at the ingenuity of its designers and builders. There is true artistry in bridge design, and aspiring civil engineers should have some familiarity with the masterpieces of art and architecture if they are to pursue careers involving the design of major structural landmarks.
Seas Summer Scholars Research Blood Vessel Cells, Cytoskeleton
Via Hofstra University | August 6, 2014This summer, Dr. Sina Rabbany, Hofstra’s Jean Nerken Professor of Engineering and Director of the Bioengineering Program, is working with a talented group of students from varied age groups and educational backgrounds to continue research on examining the role of biomechanical forces on endothelial cells (EC) – the cells that make up the structure of blood vessels. This research is supported by the Dean’s Fund of the School of Engineering and Applied Sciences, using a donation made by Mr. Paul Saueracker ’78, CEO, Minerals Technologies (retired).
The hope is that by creating cell culture conditions that maintain the cells in a more physiologic state, the ECs may be more accurately characterized. Two of the Saueracker Scholars are rising juniors and bioengineering majors, Nickolas Boroda from Massapequa, NY, and Pierre Llanos, from Ocenaside, NY. The third beneficiary of the research fund is Andrew Wong, from Manhasset, NY, a graduate of Tulane University, who is serving as a design engineer for the devices created to study the ECs.
Not All Blood Vessels Are Created Equal: Groundbreaking Research of Endothelial Cells May Someday Lead to Elimination of Organ Transplants
Via Hofstra University | October 25, 2013Research by a group of scientists, including Dr. Sina Rabbany, Hofstra’s Jean Nerken Professor of Engineering and Director of the Bioengineering Program, and his colleagues from Weill Cornell Medical College, found that damaged or diseased organs may someday be restored with an injection of endothelial cells – the cells that make up the structure of blood vessels. This could someday eliminate the need for donated organs and transplants. The findings of this research were published in Stem Cell Journal.
The studies show that endothelial cells drive regeneration because they adapt and learn how to act like an organ-specific blood vessel. Previously it was thought that blood vessels were the same throughout the body. This is not the case. Depending on the organ, the endothelial cells in the blood vessels vary in shape and function. According to Dr. Rabbany, the endothelial cells are versatile, so they can be transplanted into different tissues, become educated by the tissue, and acquire the characteristics of the native endothelial cells.
Blood Vessel Cells Can Repair, Regenerate Organs, Say Weill Cornell Scientists
Via Weill Cornell Medical College | October 8, 2013Damaged or diseased organs may someday be healed with an injection of blood vessel cells, eliminating the need for donated organs and transplants, according to scientists at Weill Cornell Medical College.
In studies appearing in recent issues of Stem Cell Journal and Developmental Cell, the researchers show that endothelial cells — the cells that make up the structure of blood vessels — are powerful biological machines that drive regeneration in organ tissues by releasing beneficial, organ-specific molecules.
They discovered this by decoding the entirety of active genes in endothelial cells, revealing hundreds of known genes that had never been associated with these cells. The researchers also found that organs dictate the structure and function of their own blood vessels, including the repair molecules they secrete.
New Study Shows Reprogrammed Amniotic Fluid Cells Could Treat Vascular Diseases
Via Weill Cornell Medical College | October 18, 2012A research team at Weill Cornell Medical College has discovered a way to utilize diagnostic prenatal amniocentesis cells, reprogramming them into abundant and stable endothelial cells capable of regenerating damaged blood vessels and repairing injured organs.
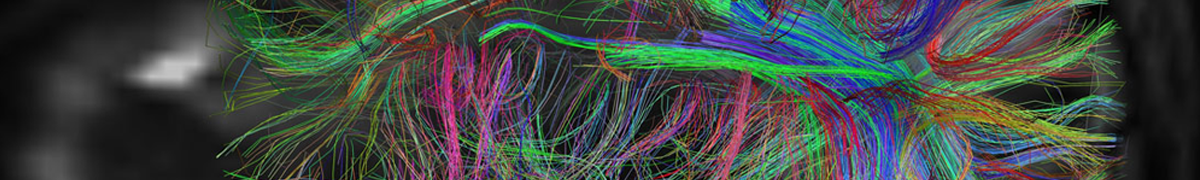
Blood vessel composed of new endothelial cells, created from reprogrammed amniotic fluid-derived cells
Their study, published online today in Cell, paints a picture of a future therapy where amniotic fluid collected from thousands of amniocentesis procedures yearly, during mid-pregnancy to examine fetal chromosomes, would be collected with the permission of women undergoing the test. These cells, which are not embryonic, would then be treated with a trio of genes that reprogram them quickly into billions of endothelial cells — the cells that line the entire circulatory system. The new endothelial cells could be frozen and banked the same way blood is, and patients in need of blood vessel repair would be able to receive the cells through a simple injection.
Lung Regeneration Closer to Reality With New Discovery by Weill Cornell Medical College Researchers
Via Weill Cornell Medical College | October 28, 2011Researchers at Weill Cornell Medical College say they have taken an important step forward in their quest to “turn on” lung regeneration — an advance that could effectively treat millions of people suffering from respiratory disorders.
In the Oct. 28 issue of the journal Cell, the research team reports that they have uncovered the biochemical signals in mice that trigger generation of new lung alveoli, the numerous, tiny, grape-like sacs within the lung where oxygen exchange takes place. Specifically, the regenerative signals originate from the specialized endothelial cells that line the interior of blood vessels in the lung.
While it has long been known that mice can regenerate and expand the capacity of one lung if the other is missing, this study now identifies molecular triggers behind this process, and the researchers believe these findings are relevant to humans.
Specialized Blood Vessels Jumpstart and Sustain Liver Regeneration
Via Weill Cornell Medial College | November 11, 2010The liver’s unique ability among organs to regenerate itself has been little understood. Now Weill Cornell Medical College scientists have shed light on how the liver restores itself by demonstrating that endothelial cells — the cells that form the lining of blood vessels — play a key role.
The results of their study are published today in the online edition of the journal Nature, with a companion study in the Oct. 24 issue of Nature Cell Biology describing how endothelial cells are activated to initiate organ regeneration.
It has long been known that endothelial cells passively conduct blood, passing oxygen, nutrients and metabolic waste to and from tissues through capillary walls. However, in studies published in recent years, the Weill Cornell researchers have demonstrated that endothelial cells actively influence the self-renewal of certain stem cell populations and the regeneration of tissue. Now, these scientists have uncovered the endothelial cells’ “instructive role” in liver regeneration. Further, the researchers believe that in the coming years it will be possible to facilitate healing damaged livers by transplanting certain types of endothelial cells with liver cells.
Hofstra Professor’s Research May Lead to New Treatments of Cardiovascular Disease, Stroke
Via Hofstra University | February 1, 2010A team of scientists, including Hofstra bio-engineering professor Sina Rabbany, have devised a new method of turning embryonic stem cells into durable blood-vessel-forming cells, a breakthrough with potential to dramatically improve the treatment of diseases ranging from stroke to cardiovascular disease.
The new technique, outlined in a study that appears in the Jan. 17, 2010 online issue of Nature Biotechnology, increases by 40-fold the number of blood vessel-forming cells – or endothelial cells – that can be generated from stem cells. The ability to generate vast quantities of endothelial cells addresses a significant hurdle in stem-cell research – namely that scientists had previously struggled to create the many millions of blood-vessel-forming cells needed for effective treatment therapies.
Dr. Rabbany said the research “may serve as a giant step toward repairing damaged vessel networks, such as one might find after burns, heart attacks or stroke.
New Way to Generate Abundant Functional Blood Vessel Cells From Human Stem Cells Discovered
Via Weill Cornell Medical College | January 20, 2010In a significant step toward restoring healthy blood circulation to treat a variety of diseases, a team of scientists at Weill Cornell Medical College has developed a new technique and described a novel mechanism for turning human embryonic and pluripotent stem cells into plentiful, functional endothelial cells, which are critical to the formation of blood vessels. Endothelial cells form the interior “lining” of all blood vessels and are the main component of capillaries, the smallest and most abundant vessels. In the near future, the researchers believe, it will be possible to inject these cells into humans to heal damaged organs and tissues.
The new approach allows scientists to generate virtually unlimited quantities of durable endothelial cells — more than 40-fold the quantity possible with previous approaches. Based on insights into the genetic mechanisms that regulate how embryonic stem cells form vascular endothelial cells, the approach may also yield new ways to study genetically inherited vascular diseases. The study appears in the advance online issue of Nature Biotechnology.
A Bountiful Harvest Offers Promise for Regenerating Blood Vessels | Howard Hughes Medical Institute (HHMI)
Via Howard Hughes Medical Institute | January 17, 2010Howard Hughes Medical Institute (HHMI) researchers have devised a new method that increases the number of blood vessel-forming cells they can make from human embryonic stem cells. The advance could improve the odds for successful cell-based therapies to treat heart disease or stroke, and might also aid engineering of artificial organs.
 AIMBE
AIMBE
